What if I told you that increasing annual influenza vaccination of the elderly is associated with increased influenza-related death in the elderly?
What if I told you that annual influenza vaccination can make you more susceptible to influenza-like illness?
What if I told you that deploying leaky influenza vaccines (into either humans or poultry flocks) will accelerate the evolution of vaccine-resistant influenza viruses?
What if I told you that the real problem with influenza virus-associated death in the elderly is due to the aging of their immune systems (immunosenescence)?
What if I told you that most of the 1918 “Spanish Flu” deaths could have been prevented if (antibacterial) antibiotics had been available?
What if I told you that most countries do not recommend population-wide annual influenza vaccination?
What if I told you that USG annual influenza vaccination policy is influenced by a desire to support and maintain influenza manufacturing capacity?
What if I told you that most of what you have been told about annual influenza vaccination is propaganda?
I have written about most of these issues before, but not as bluntly as I do here. I thank and acknowledge Substack author Sharyl Atkinson for triggering me to write in a more frank and plain style with the following Substack essay, which provides additional reporting and context for what I write below:


Background and Bona Fides
I am an expert on influenza and influenza vaccine development. I once held the position of Director, Clinical Influenza Vaccine Development at Solvay (now Abvie) Pharmaceuticals under an approximately $350 million US Government BARDA contract. I have won and/or managed hundreds of millions of dollars in federal contracts for development of more effective influenza vaccines. I have spoken (by invitation) on innovative influenza vaccine development at the World Health Organization in Geneva. I also have lost clients and at least one job for just (internally) discussing the issue of influenza vaccines and “original antigenic sin”—which is a forbidden topic among influenza vaccine manufacturers and the scientific-medical guild that supports this industry.
I fully expect this essay to be weaponized against me by the likes of Media Matters and Government (and Pharma)-sponsored corporate media. They already demean me as a spreader of misinformation during the COVIDcrisis, and as the vaccine—developing vaccine technology innovator who is an anti-vaxxer—and both sides (pro-vax and anti-vax) have called me a mass murderer for speaking truth to power. How much nastier can they get?
Damn the torpedos, full speed ahead.
If the “Make America Healthy Again” movement is to succeed, it must be willing to look the data in the face and not flinch from the obvious conclusions. It must be willing to examine long-standing assumptions and reconsider established public health policies. Because many, if not most US citizens are not healthy, and our average lifespan is declining. We are (on average) fat, suffering from an epidemic of chronic disease, and our massive levels of spending on “public health” and “healthcare” are not fixing the problem.
Let’s examine these influenza vaccine heresies one by one.
Increasing Annual Influenza Vaccination of the Elderly Is Associated with Increased Influenza-Related Death in the Elderly
The main issue with influenza is “influenza-like” disease and death (morbidity and mortality) in the elderly, and in those with significant pre-existent conditions. In other words, upper-respiratory viral pneumonia on top of certain other conditions can tip the sick and elderly over the edge. This is similar to the issue of disease and death from SARS-CoV-2 (Covid) primarily happening to people that had other health problems—one of those other health problems being old age in general. People mostly died WITH Covid, not necessarily FROM Covid—same with influenza. And by the way, “influenza-like illness” is a grab bag.
For purposes of public health data analysis, in most cases, upper respiratory viral disease is typically assumed to be due to influenza virus. The inconvenient fact is that there are many viruses and other pathogens that cause “influenza-like” illness, disease, and death. Influenza viruses (types A and B), respiratory syncytial virus (RSV), parainfluenza viruses, rhinoviruses, coronaviruses, adenoviruses, metapneumovirus, group A streptococcus, mycoplasma, chlamydia, and Bordetella pertussis. The most common cause of “walking pneumonia” is mycoplasma—which is not really a virus! From this brief explanation, you can see that the cited “deaths from Influenza” data are usually inflated, just like “deaths from Covid” were.
There is a clinical saying, that “pneumonia is the old man’s friend.” Meaning that when you are old, feeble, and suffering from various chronic disease conditions, a quick death associated with pneumonia (often with sepsis complications) can relieve you from pain and suffering.
Of course now we have government-supported MAID (medical assistance in dying) in many countries which provides an even easier, less traumatic exit for those who are not concerned about the theologic, ethical, practical, or conflict-of-interest implications of state-sponsored medical suicide.
All market-approved influenza vaccines include or encode proteins (antigens) from both Influenza A and Influenza B. The specific strains of A and B included in a given year’s vaccine preparation vary from year-to-year based on recommendations from a WHO working group that looks at Northern and Southern Hemisphere trends modeled based on preceding year strain monitoring data.
Now you have the background to better appreciate this bombshell “peer-reviewed” paper.
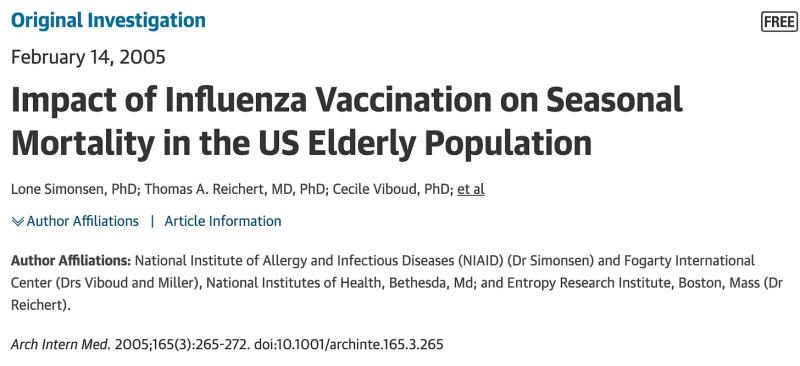
Abstract
Background: Observational studies report that influenza vaccination reduces winter mortality risk from any cause by 50% among the elderly. Influenza vaccination coverage among elderly persons (> or =65 years) in the United States increased from between 15% and 20% before 1980 to 65% in 2001. Unexpectedly, estimates of influenza-related mortality in this age group also increased during this period. We tried to reconcile these conflicting findings by adjusting excess mortality estimates for aging and increased circulation of influenza A(H3N2) viruses.
Methods: We used a cyclical regression model to generate seasonal estimates of national influenza-related mortality (excess mortality) among the elderly in both pneumonia and influenza and all-cause deaths for the 33 seasons from 1968 to 2001. We stratified the data by 5-year age group and separated seasons dominated by A(H3N2) viruses from other seasons.
Results: For people aged 65 to 74 years, excess mortality rates in A(H3N2)-dominated seasons fell between 1968 and the early 1980s but remained approximately constant thereafter. For persons 85 years or older, the mortality rate remained flat throughout. Excess mortality in A(H1N1) and B seasons did not change. All-cause excess mortality for persons 65 years or older never exceeded 10% of all winter deaths.
Conclusions: We attribute the decline in influenza-related mortality among people aged 65 to 74 years in the decade after the 1968 pandemic to the acquisition of immunity to the emerging A(H3N2) virus. We could not correlate increasing vaccination coverage after 1980 with declining mortality rates in any age group. Because fewer than 10% of all winter deaths were attributable to influenza in any season, we conclude that observational studies substantially overestimate vaccination benefit.
In other words, according to this study, natural immunity acquired by influenza infection works to prevent future “influenza-related” deaths in the elderly. Vaccination to a specific influenza A virus strain (H1N1) does not improve on natural immunity to that specific influenza A virus strain, and, on average, increased influenza vaccine uptake increases all-cause “influenza-related” death (mortality) in the key age group of the elderly, where most of the “influenza-related” deaths occur.
This is not what we are told, and it calls into question whether we are wasting a lot of money and effort (and propaganda) to dose the entire population with injectable products that DO have risks. Whatever those risks are, how serious, how frequent, in what age and risk factor groups we do not really know because this is (basically) a forbidden topic of inquiry.
Maybe MAHA should think this through again?
Annual Influenza Vaccination Can Make You More Susceptible to Influenza-Like Illness
The issue here was originally described as “original antigenic sin,” but now the more politically correct term is “immune imprinting.”


The term “original antigenic sin” (OAS) was first used in the 1960s to describe how one’s first exposure to influenza virus shapes the outcome of subsequent exposures to antigenically related strains.
The “Cliff Notes” version here is that if you get “boosted” every year with a suboptimal influenza “vaccine,” it sets your immune system up to be focused on last year’s virus rather than to being better able to respond to tomorrow’s strain. This is a form of immune system bias. This can make it so that you are less able to fight off newly evolved strains.
Maybe MAHA should think this through again?
This leads directly to the next point—
Deploying Leaky Influenza Vaccines (into either Humans or Poultry Flocks) Will Accelerate the Evolution of Vaccine-Resistant Influenza Viruses
“Leaky vaccine” is industry jargon for partially effective products intended to prevent infection, replication, spread, and disease caused by what you are “vaccinating” against. As can be inferred from the initial paper cited above, the current gold standard for “effectiveness” in influenza “vaccines” is natural infection. And natural infection is not completely effective. Otherwise, we would all get one influenza A infection and one influenza B infection when we are children, and that would confer lifelong protection against all influenza viruses.
Influenza virus continues to circulate in humans (and birds, and other animals) because it is partially able to evade immune responses generated by prior infections in these animals. And it continually evolves (“drifts and shifts”) to better evade those responses.
The less effective a “vaccine” product is at preventing infection and replication of an infectious pathogen, the more likely widespread dosing with that product will select for pathogens that are more ‘vaccine resistant.” This, plus the fact that “Bird flu” is endemic in wild birds, is why we CANNOT vaccinate our way out of the risk posed by “Bird flu” to either poultry flocks or other animals. If we vaccinate commercial flocks (say ducks or chickens) with a partially effective vaccine, what we will get is “bird flu” that has evolved to become more resistant to that vaccine. Furthermore, “vaccination” that partially suppresses disease without preventing replication and spread of the virus will actually increase the risk of crossover into the humans that handle those birds, because they will have a harder time recognizing a sick flock and so will be less likely to take precautions to not get infected themselves.
You cannot “vaccinate” your way out of an outbreak of influenza (or a coronavirus, for that matter) with an imperfect “vaccine,” and if you try you will only make matters worse. This is a fundamental truth. All influenza vaccines to date are imperfect because we have not learned how to make a “vaccine” that is sterilizing and works better than natural infection.
Maybe MAHA should think this through again?
The Real Problem with Influenza Virus-Associated Death in the Elderly is Due to the Aging of Their Immune Systems (Immunosenescence)
Yes, as we age, for some reason, our immune systems age with us. Immunology scientists like to create their own words and language for everything in their field (I like to call it “immunobabble”); usually coining words and phrases that include some part of the term ‘immunology.” So it is no surprise that when they encountered the reality that immune systems become less effective as they age, they coined a term merging “immuno”—and a fancy term for aging—“senescence.”
“Infection susceptibility, poor vaccination efficacy, age-related disease onset, and neoplasms are linked to innate and adaptive immune dysfunction that accompanies aging (known as immunosenescence).”
Immunosenescence: molecular mechanisms and diseases
Nature Medicine, Sig Transduct Target Ther 8, 200 (2023). https://doi.org/10.1038/s41392-023-01451-2
If we are going to shift the NIH research enterprise to focusing on promoting health rather than preventing and treating specific diseases, including influenza-like illness, maybe we should focus the hundreds of millions of dollars being spent on developing an mRNA vaccine for “bird flu” to understanding the causes of immunosenescence. Because it looks like many of those causes are also involved in a wide range of other diseases—including cancer.
During aging, organisms tend to develop a characteristic inflammatory state that expresses high levels of pro-inflammatory markers, termed inflammaging. This chronic inflammation is a typical phenomenon linked to immunosenescence and it is considered the major risk factor for age-related diseases. Thymic involution, naïve/memory cell ratio imbalance, dysregulated metabolism, and epigenetic alterations are striking features of immunosenescence. Disturbed T-cell pools and chronic antigen stimulation mediate premature senescence of immune cells, and senescent immune cells develop a proinflammatory senescence-associated secretory phenotype that exacerbates inflammaging.
See this prior substack for more information.
Most of the 1918 “Spanish Flu” Deaths Could Have Been Prevented if (Antibacterial) Antibiotics Had Been Available
I have spoken about this many times in person and on podcasts. The 1918 “Spanish Influenza” outbreak story that is so often trotted out as a source of fear to support universal influenza vaccination policies is a false narrative. This event was the most lethal single infectious disease event in modern history. But were the deaths actually due to influenza infection?
The 1918 pandemic appeared in almost all inhabited places on Earth, causing, over the course of a year, symptomatic disease in approximately one-third of the world’s population, with evidence that a significant percentage had been asymptomatically or subclinically infected (Philip and Lackman 1962; Masurel 1976; Dowdle 1999; Taubenberger et al. 2001). The majority of people presenting with clinical illness in the 1918 pandemic had typical, self-limiting influenza, but a disproportionate number developed lower respiratory involvement and died of the consequences of pneumonia (Morens et al. 2008).
The 1918 Influenza Pandemic and Its Legacy
Cold Spring Harb Perspect Med. 2020 Oct;10(10):a038695.
Most people recovered from their influenza virus infection. What killed them was a secondary bacterial pneumonia—because antibiotics had yet to be discovered! And, to a lesser extent, overdosing on the new wonder drug “aspirin” contributed to the deaths. Mask use may have also played a role.
If adequate doses of antibiotics had been available at the time, the deaths would have been avoided. Currently, almost the entire US supply of antibiotics is manufactured in India and China. Instead of massive investments in the development of new mRNA vaccines for influenza strains, when we already have more traditional vaccines, perhaps we should invest in domestic US antibiotic research and manufacturing capacity?
Maybe MAHA should think this through again?
Most Countries Do Not Recommend Population-Wide Annual Influenza Vaccination
This point does not require much of an explanation. It is either true or false. The question is whether it is really necessary to maintain the massive investment in treasure, labor, and propaganda to sustain an annual influenza vaccination program that does not achieve its objective of protecting the elderly from death and disease caused by influenza-like illness, of which only a subset is actually caused by influenza viruses? Note that not even the WHO recommends influenza vaccination for the entire population.
The WHO recommends annual influenza vaccination to prevent influenza illness in high-risk groups. Little is known about national influenza immunization policies globally.
Of 194 WHO Member States, 115 (59%) reported having a national influenza immunization policy in 2014. Among countries with a national policy, programmes target specific WHO-defined risk groups, including pregnant women (42%), young children (28%), adults with chronic illnesses (46%), the elderly (45%), and health care workers (47%). The Americas, Europe, and the Western Pacific were the WHO regions that had the highest percentages of countries reporting that they had national influenza immunization policies.
Maybe MAHA should think this through again?
USG Annual Influenza Vaccination Policy Is Influenced by a Desire to Support and Maintain Influenza Manufacturing Capacity
I have previously been “fact-checked” as spreading “misinformation” for saying this, but having participated in CDC briefings and various discussions within the federal government on this topic, I can assure you that this is a key consideration. If one accepts the hypothesis (propaganda narrative) that the Spanish flu was caused by H1N1, and that if a similarly lethal and infectious influenza virus arises again, then it is absolutely essential and in the interests of national security to guarantee that sufficient quantities of influenza vaccine (rather than antibiotics to treat secondary pneumonia) must be available on short notice.
The problem is that you cannot build and mothball an influenza vaccine manufacturing facility for future use. Manufacturing influenza vaccine is a specialty requiring maintenance of ongoing production and highly skilled personnel. If this is the mandate, then you must maintain “warm base manufacturing.” In other words, you have to keep making influenza vaccines on a regular basis. And if you are going to make it, and have the enterprise be economically sustainable, the USG, CDC, and BARDA have determined that you need to have a market for the product. From this, you can understand why all of the marketing, propaganda, subsidies, etc. for manufacturing influenza vaccine and universally dosing every man, woman, and child on an annual basis is thought essential.
But is the risk real? And is this sufficient justification for the influenza vaccine mandates and propaganda?
Maybe MAHA should think this through again?
In Conclusion, Most of What You Have Been Told about Annual Influenza Vaccination Is Propaganda.
The budget for public health is not and should not be unlimited. And the proper role of government is not to try to ensure equality of health outcomes. If anything, government should seek to enable equality of health promotion opportunities. Citizens should have the opportunity to select what ways they choose to promote their own health, and should have access to ALL of the information necessary for them to make informed decisions regarding their selections.
Contrary to Media Matters and Wikipedia, I am not an anti-vaxxer, nor a vaccine denier. Rather, I am an advocate for sound, well-justified medical practices, decentralized decision-making involving partnerships between physicians and patients, and rigorous compliance with fundamental principles of medical ethics including the right of patients to require informed consent for medical procedures—and “vaccination” is a medical procedure.
As an expert in influenza vaccine development and practice, I do not endorse current US “universal influenza vaccination” mandates, policies, and practices, nor the propaganda routinely deployed to enforce these policies.
Making America Healthy Again will require respect for patients and their own personal bodily autonomy (as well as their children’s). There must be a recognition that much of what is assumed about vaccine efficacy and safety is NOT “settled science,” and that the proper mechanism for medical decision-making is not by top-down mandates. The more correct mechanism should involve decisions made on a person-by-person basis with the assistance and support of unbiased health advocates and coaches—otherwise known as physicians and allied medical care providers.
Do you believe in fate, Neo?
No. Why not?
Because I don’t like the idea that I am not in control of my own life.
Maybe MAHA should think this through again?
Republished from the author’s Substack
Join the conversation:


Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.