The two narratives about the Covid-19 pandemic continue to clash as evidence mounts about the actual outcomes of the extraordinary strategies governments deployed to try and contain the epidemic. Has the emerging evidence vindicated the decisions governments have been making over the past three years? In particular, were they ethically justified in imposing harsh mandates on their populations?
At the outset, of course, there was actually no evidence whatsoever that lockdowns would work – zero. Because they had never been tried before, there was no accumulated knowledge to go on.
There was only theory and modelling, and it is important to stress that modelling is not empirical evidence.
And even the initial modelling did not show that universal lockdowns were the preferable strategy. As I have pointed out before, Neil Ferguson’s infamous ‘Report 9’ actually shows the lowest epidemic curve resulting from a mix of measures including confinement only for the over 70s.
Interestingly, a team from the University of Edinburgh has run a version of the same model, with some modifications (especially, ‘We also count deaths in all waves, not just the first’) and arrived at similar conclusions. Table 3 in their report summarises counterintuitive findings, including that:
adding school closures to a scenario with case isolation, household quarantine, and social distancing in people older than 70 years would increase the total number of deaths across the full simulation. Moreover, it shows that social distancing in those over 70 would be more effective than general social distancing.
Then they went further, and found that: ‘Stronger interventions…are associated with suppression of the infection such that a second wave is observed once the interventions are lifted:’
When the interventions are lifted, there is still a large population who are susceptible and a substantial number of people who are infected. This then leads to a second wave of infections that can result in more deaths, but later. Further lockdowns would lead to a repeating series of waves of infection unless herd immunity is achieved by vaccination, which is not considered in the model.
In summary: ‘Postponing the spread of covid-19 means that more people are still infectious and are available to infect older age groups, of whom a much larger fraction then die.’ This is represented in their Figure 1, in which the first five scenarios are the same ones presented by Ferguson’s Report 9, with another three scenarios showing the second (or later) wave scenarios with either general social distancing or social distancing for the over 70s.
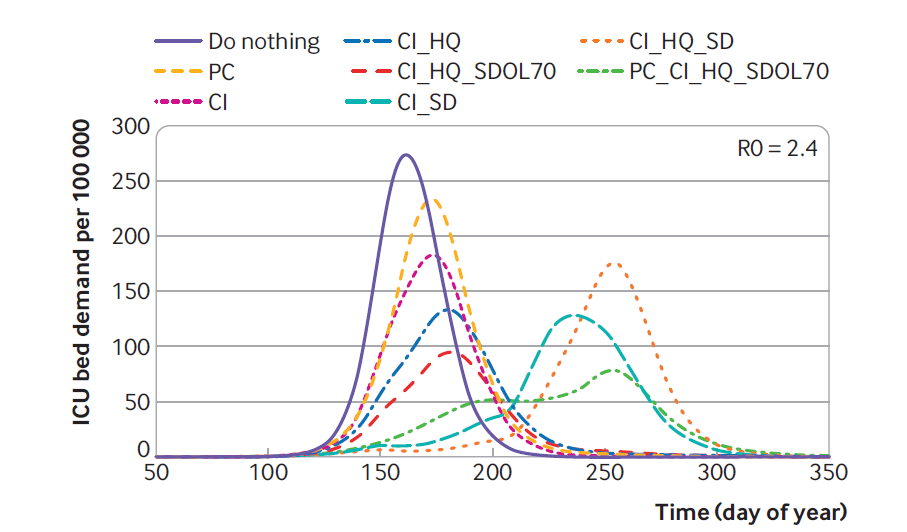
Key: ICU =intensive care unit; PC=place closures; CI =case isolation; HQ=household quarantine; SDOL70=social distancing of over 70s; SD=general social distancing.
None of this modelling might be reliable (see below), but the point is: the same model that launched the lockdowns also indicates that the medium-term outcomes might be unfavourable, so experimenting with lockdowns was a dangerous experiment, a leap in the dark. Governments had no idea whether the emergency measures would increase or decrease even COVID-19 mortality, let alone mortality overall, in the medium term.
This is serious, as evidence of the ‘collateral damage’ or adverse effects from lockdowns has been mounting.
The World Bank estimated that the combined effects of the pandemic itself and lockdowns led to 97 million more people being in poverty in 2020 than the previous year. It is likely that most of these adverse effects derived from the lockdowns, as the poorer countries predominantly have a younger population that are less susceptible to the disease. They were made to endure harsh interventions that were not remotely justifiable given their lower risk profile.
Li et al. reviewed 256 studies worldwide on the effects of lockdowns on older people, children/students, low-income populations, migrant workers, people in prison, people with disabilities, sex workers, victims of domestic violence, refugees, ethnic minorities, and people from sexual and gender minorities and summarised their findings:
We show that prolonged loneliness, mental distress, unemployment, income loss, food insecurity, widened inequality and disruption of access to social support and health services were unintended consequences of physical distancing that impacted these vulnerable groups and highlight that physical distancing measures exacerbated the vulnerabilities of different vulnerable populations.
We can be sure that increased unemployment and mental stress will increase the burden of illness for years to come.
Townsend and Owens confirmed that Lockdowns Crush Mental Health and Wellbeing in Young People, finding that the experience of depression among young people during lockdowns was 55 percent higher than before the pandemic.
Robertson et al. examined the effect of reduced maternal and child health interventions and found:
Our least severe scenario (coverage reductions of 9.8–18.5% and wasting increase of 10%) over 6 months would result in 253,500 additional child deaths and 12,200 additional maternal deaths. Our most severe scenario (coverage reductions of 39.3–51.9% and wasting increase of 50%) over 6 months would result in 1,157,000 additional child deaths and 56,700 additional maternal deaths.
There were dire warnings that COVID-19 would cut swathes through the population of the Indian slums, where people live on top of each other. Malan et al. found that 54 percent of the population in the slums of Mumbai tested positive, as compared with 16.1 percent in the ‘non-slums.’ But they also found that the infection fatality rate in the slums was only 0.076 percent, as compared with 0.263 percent in the non-slums.
This throws the whole social distancing hypothesis to the ground. The slum-dwellers had lower mortality than their more well-off neighbours. The authors comment drily: ‘This stark variation in prevalence within wards also highlights the importance of geographic variation for epidemiological modelling and policy discussions of herd immunity.’ Indeed, perhaps if we want a population to get to herd immunity as quickly as possible, we should herd them all together, not keep them apart!
The slum-dwellers were the lucky ones – the Indian lockdowns and associated panic thrust untold numbers of others out of the cities and back to their home villages. As Jesline et al. comment: ‘The concept of social distancing bears no meaning for the migrants because of the persistence of even more pressing and nagging problems of insecurity and hunger.’
These papers make it evident that the poor endured multiple traumas and risks, and there is little reason to believe that they benefited.
What happened in rich countries?
Here is a graph from the Australian Bureau of Statistics (ABS) showing all-cause and excess mortality over the period of six years until late 2020 in my home state of Victoria:
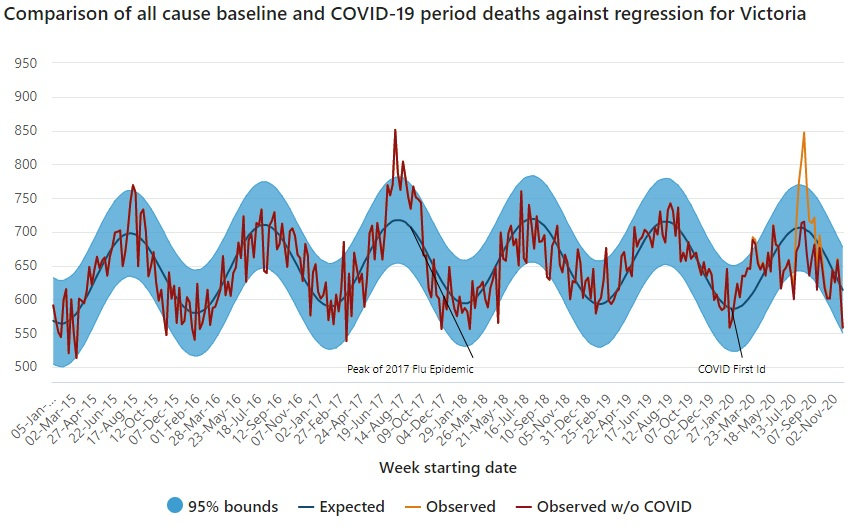
There are two striking features in this figure.
First, the 2020 peak was slightly lower than the peak of the 2017 influenza epidemic. But 2020 was meant to be the first wave of a once-in-a-hundred years pandemic comparable to the influenza pandemic of 1918. Yet 2020 all-cause mortality looks to be merely at the top of the expected range.
Second, the epidemic curve bears no relationship to what was predicted by the ICL or local modelling. There is no sign of the curve being flattened, although Melbourne had the world’s longest (cumulative) lockdown. In fact, the curve is actually sharper than the one in 2017. The modelling is comparative, so you would expect that the comparison between the ‘do nothing’ curve and the intervention curve would be transferable across locations, if the theoretical assumptions have any validity. The Victorian epidemic curve looks like the ‘do nothing’ curve, despite the harshest interventions ever attempted.
We can also benchmark against the neighbouring state of New South Wales. The graphs and tables here show that New South Wales had lower excess deaths in each year of the pandemic, despite taking a more cautious approach to lockdowns. They also show that excess mortality in Australia overall increased in 2021 and 2022 as government interventions went further. Now 2021 was the year of ‘vaccination +’ (both lockdowns and vaccinations), while in 2022 governments backed off from lockdowns and relied only on vaccination. Mortality increased again.
Case studies of island nations which were relatively isolated during the lockdowns are useful. For example, Iceland also had a more cautious approach compared with New Zealand, following a mitigation strategy instead of New Zealand’s pursuit of elimination. Local experts who are making their case out to the New Zealand COVID-19 inquiry opine: ‘Iceland’s success at keeping COVID cases and deaths relatively low without the use of stringent restrictions led to the question of whether New Zealand could have achieved similar results without a border closure and lockdowns.’ Inevitably they fall back on their modelling to argue that New Zealand could have achieved better outcomes if it had imposed lockdowns earlier, even though New Zealand went hard only four days after the pandemic was declared on 11 March 2020.
So, the push is on to impose lockdowns the same day as a pandemic is declared (preferably earlier!), at a time when nothing is known about its characteristics and relevant risk factors. And this will again be done on the basis of modelling, which is not evidence.
The lockdown hypothesis is not falsifiable, it seems. Whatever the empirical outcomes, the experts prescribe more lockdowns. But most COVID-19 inquiries will accept the need for lockdowns to be imposed more quickly. This will only lead to governments being trigger-happy and taking action too early over outbreaks that do not spread so much.
The Scottish COVID-19 inquiry took a ‘novel’ approach by commissioning a review of the evidence within the framework of evidence-based medicine, which discriminates between types of evidence, some of which are more reliable than others. Most of the academic papers that find in favour of the interventions are based on ‘observational’ studies, which are prone to bias arising from the relatively uncontrolled population samples they select, rather than the more reliable and highly-rated randomised controlled studies (RCTs).
Dr Croft’s report is rigorous and systematic. The overall findings:
- In 2020 there was scientific evidence to support the use of some of the physical measures (e.g. frequent handwashing, the use of PPE in hospital settings) adopted against COVID-19.
- For other measures (e.g. face mask mandates outside of healthcare settings, lockdowns, social distancing, test, trace and isolate measures) there was either insufficient evidence in 2020 to support their use – or alternatively, no evidence; the evidence base has not changed materially in the intervening three years.
- It has been argued that the restrictive measures introduced during the COVID-19 pandemic resulted in individual, societal and economic harm that was avoidable and that should not have occurred.
- It remains unclear as to whether or not COVID-19 vaccination has resulted in fewer deaths from COVID-19.
The world’s governments embarked on a grand experiment in March 2020, deploying harsh and untried measures on whole populations, without any evidence or insufficient evidence that they would succeed. The idea that total lockdowns would lead to better outcomes was a hypothesis, a hypothesis that needed to be tested before it was deployed in a population at large. Governments should have commissioned RCTs to test the hypotheses that lockdowns and the other non-pharmaceutical interventions would improve overall outcomes. They never did so.
RCTS were conducted for the vaccines, but only a few months of data were collected before they were unblinded and governments started authorising and even mandating the vaccines. This was well before a complete picture of their adverse effects could emerge. And the trials did not establish that the vaccines could save lives, or even ‘slow the spread.’
But Fraiman et al. analysed the data from the mRNA trials of both the Pfizer and the Moderna vaccines and found that: ‘Combined, there was a 16% higher risk of serious adverse events in mRNA vaccine recipients.’ They called for ‘formal harm-benefit analyses’ to be undertaken, but this fell on deaf ears. The vaccine RCTs fell far short of best practice, and governments should have recognised their limitations when framing policy.
The need to undertake rigorous and probing trials of unproven interventions is the basis of medical research ethics, which I am conscious of as the chair of the Human Research Ethics Committee of a small medical institute. The Nuremberg Code requires that participants in an experiment, the outcome of which is unknown, must give their voluntary consent with full knowledge of the possible risks. This never happened. Also ‘the experiment should be so conducted as to avoid all unnecessary physical and mental suffering and injury.’ Insufficient or no consideration was given to minimising suffering. These principles are amplified in the Helsinki Declaration.
The defence would argue that the threat was so great, governments could not wait to conduct RCTs. But without RCTS, they did not know (and still do not know) whether the benefits outweigh the costs. It is not justifiable in a public health emergency to deploy measures with massive adverse effects on the grounds that they might work in theory, or in virtual reality (modelling). Ioannidis and colleagues have put forward forceful critiques of forecasting and modelling here and here (‘Effect estimates of COVID-19 non-pharmaceutical interventions are non-robust and highly model-dependent’).
The strategies must pass the legal test of necessity. A harsher measure should not be deployed if a more moderate measure would work as well. Indeed, this is written into the Victorian public health legislation. But Bendavid et al. analysed the data from 10 countries and found that harsher measures did not have any significant beneficial effect on case growth compared to more moderate measures.
Governments must select the least harmful measures that can reasonably be expected to achieve the desired outcome overall, which should be lowering excess deaths not just in the short term, but in the medium and long term. And lowering deaths from one particular illness is not defensible if it might increase deaths from other illnesses, for example through deferred health and medical appointments during lockdowns resulting in serious health conditions not being picked up early enough.
In embarking on this grand experiment governments had no idea what they were doing. They recklessly breached all known codes of medical ethics and the principle of necessity apparently without even considering them. They did not consider other tenable strategies such as allowing herd immunity to spread in the younger age groups while focussing on protecting the older age groups. Multiple red flags were thrown up, but governments drove straight past them and simply ignored any evidence of harms and failed to make any attempt to optimise the policies and minimise harms as much as possible. This represents the greatest failure of public health ethics in recorded history.
This is no conspiracy theory. My working hypothesis is that everyone concerned thought they were doing the right thing. But the charge of criminal negligence should be considered given the huge numbers of people who have suffered adverse effects from these measures unnecessarily and out of all proportion to their risk from COVID-19.
Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.