The combined efforts of the media and “expert” hive mind have created a singular acceptable public viewpoint in response to normal respiratory virus season: Get vaccinated, or else.
That sentiment was shared, simply and profoundly, by President Joe Biden, who told the country in 2021 that the “unvaccinated” would suffer a winter of severe illness and death if they didn’t do what they were told. While Biden’s words were proven laughably false a few short months later, the media and their public health partners have continued down the same path of universal vaccination regardless.
They’ve just expanded it to include every single respiratory virus, along with Covid.
But what does the evidence base actually say about the efficacy of vaccinations to stop Covid, flu, or other respiratory viruses? Is there actually a justification for this extremism, this universal messaging? Or, as with so many other Covid-era policies and mandates, is it an inexcusable overreach?
Evidence Base Doesn’t Justify Respiratory Vaccine Extremism
A study from John Ioannidis, Professor of Medicine of Epidemiology and Population Health at Stanford University and one of the scientific community’s most well-respected and prolific researchers, and Dr. Vinay Prasad, a hematologist-oncologist and Professor in the Department of Epidemiology and Biostatistics at the University of California San Francisco, explored this very question.
And it’s an important one to understand and explain, considering the pressure now placed on individuals in healthcare settings across the country to “get their flu shot.” Or considering also the relentless celebrity marketing campaigns from Pfizer telling the public to get their Covid and flu shots at the same time.
The study goal was to “analyze and question” the policymaking around the importance of respiratory virus vaccines in the US.
Annual vaccination is widely recommended for influenza and SARS-CoV- 2. In this essay, we analyse and question the prevailing policymaking approach to these respiratory virus vaccines, especially in the United States.
Immediately, in their summary, they highlight one of the most important issues of how the Covid vaccinations have been handled in the US thus far.
The emergence of highly transmissible SARS-CoV-2 variants and waning vaccine-induced immunity led to plummeting vaccine effectiveness, at least against symptomatic infection, and booster doses have since been widely recommended. No further randomized trials were performed for clinically important outcomes for licensed updated boosters.
Instead of conducting actual randomized trials to assess whether updated booster shots would be more effective than the original vaccination series over time and against new variants, public health officials and regulators lowered the standard of evidence they should have required.
This means that instead of demanding high-quality evidence, the CDC, FDA, Fauci, and their partners accepted “mice immunogenicity data” instead. That laughable criterion has since been updated to include “observational studies,” but those too are prone to several issues that could easily undercut assumed results.
In both cases, annual vaccine effectiveness estimates are generated by observational research, but observational studies are particularly susceptible to confounding and bias. Well-conducted experimental studies, particularly randomized trials, are necessary to address persistent uncertainties about influenza and COVID-19 vaccines.
This uncertainty extends to the value of flu vaccines in achieving desired outcomes for those who take them. Despite years of marketing, flu shot uptake across society, even among healthcare workers, has traditionally been low. Some hospitals turned to mandatory flu vaccination to force uptake. But why?
Ioannidis and Prasad in their essay discuss a Cochrane Library review from 2018, covering the effectiveness of flu vaccines. This is before the Cochrane Library review confirmed that masks don’t work against respiratory viruses, permanently damaging their reputation amongst the pro-mask extremists. Their 2018 review was equally damaging for public health and pharmaceutical company messaging.
In 2018, Cochrane authors reviewed the evidence supporting influenza vaccines. Specifically, the authors examined 50 trials in healthy individuals under 65 years old, 41 trials in healthy children and 8 RCTs in the elderly(≥65 years) comparing influenza vaccines with placebo or no intervention. While vaccines seemingly reduce the risk of influenza-like illness over a single season (from 2.3% to 0.9% in healthy adults, from 17% to 12% for live attenuated vaccines and from 28% to 20% for inactivated vaccines in children, and from 6% to 2.4% in the elderly), data are very limited on the prevention of hospitalization, death, transmission and absence from work. For instance, vaccinated healthy adults may have a small reduction in their risk of hospital admission, but the confidence interval (CI) is wide and crosses one (relative risk [RR] 0.96, 95%CI 0.85–1.08). For the elderly, there is no data on hospitalizations, and the single randomized trial providing data for mortality and pneumonia was underpowered. Generally, most estimates in the three reviews are graded low- or moderate-certainty evidence.
Essentially, there is no high-quality data for flu vaccines specifically reducing the most important outcomes for those at the highest risk of severe illness or death. There’s merely been one randomized trial in this area, and it was “underpowered.” For healthy adults, there is quite literally zero evidence of improvement in important outcomes. And even the few results that demonstrate a benefit show marginal improvements to already low rates.
These issues are repeated in yearly estimate studies, where different groups estimate different results.
In one study, protection against influenza associated hospitalizations was 23% and 41% among adults aged 18–64 and ≥65 years, respectively. In a different study, the pattern was reversed —47% for people 18–64 years and 28% for those aged 65 and older. Moreover, given the observational nature of the data, the estimates may be even more uncertain than the typical confidence intervals may suggest.
This quite succinctly summarizes the problem: public health agencies rely on contradictory data that contain profound uncertainties, and then use that data to create mandates or policies. It’s a vicious cycle, and one that the “Experts” refuse to acknowledge at risk of undercutting their public pronouncements.
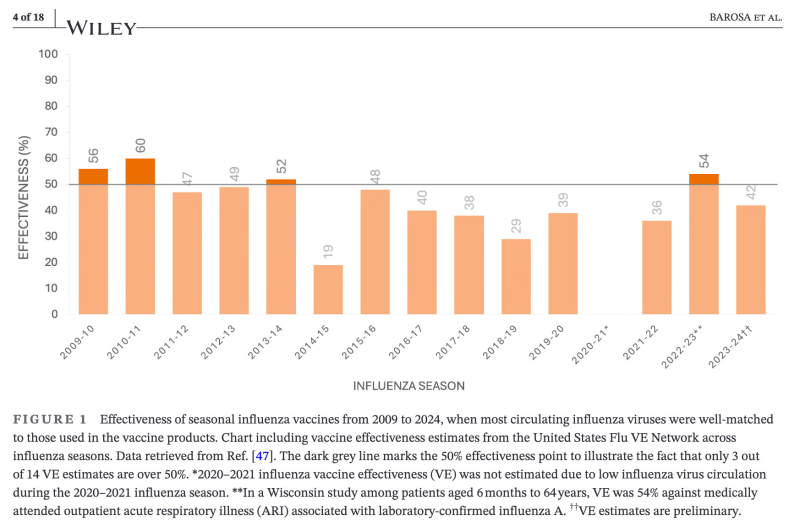
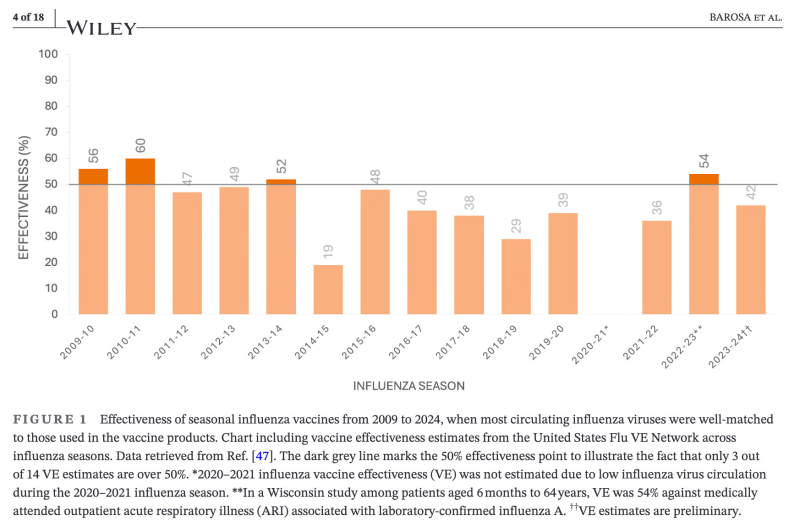
Importantly, there have been just three years in the past 14 where vaccine efficacy estimates have exceeded 50%.
So why are they pushed onto the public with such intensity?
This same problem extends to annual Covid booster doses. As Ioannidis and Prasad write, there isn’t a single randomized controlled trial that shows a benefit to booster doses in relation to severe outcomes.
No published RCT has investigated to-date the benefits of COVID-19 boosters versus no boosters on clinically relevant outcomes (severe disease, hospitalization and death),and whether any potential benefits apply the same way to different groups. It is unclear whether healthy adults, young people and even the elderly benefit from receiving boosters now that almost everyone worldwide has already been previously infected.
When the CDC has attempted to undertake an evidence review of their own to justify their promotion of yearly boosters, they’ve had little to show for it.
…several aspects of the CDC’s evidence review and conclusion raise concerns. All estimates were considered either ‘low certainty’ or ‘very low certainty’. COVID-19 was not necessarily confirmed as the cause of hospitalizations. Absolute risk was calculated using the observed risk among a single observational cohort in the available body of evidence. The absolute risk reduction is relatively low—186 fewer COVID-19 visits, 53 fewer hospitalizations and six fewer deaths per 100,000. Finally, the studies included in the review evaluated vaccine effective-ness of the previous COVID-19 vaccine.
So in order to justify yearly boosters, the CDC relied on “low” or “very low certainty” evidence, there was only one group of studied individuals used to calculate absolute risk reduction, and even that absolute risk reduction was remarkably low. In addition, they used outdated studies that examined only the original vaccination dose in a review supposedly about boosters.
Classic CDC.
This underlines the issue with how public health, experts, and the media have communicated with the public about the importance of yearly respiratory virus vaccinations. Quite simply, they have not demonstrated conclusive, high-quality evidence suggesting that getting an annual flu or Covid vaccine will meaningfully reduce the likelihood of severe illness, hospitalization, or death. Yet they’ve issued blanket recommendations for both, regardless.
All while also ignoring the importance of natural immunity in both illnesses. Even Anthony Fauci was on camera back in his intellectually honest days admitting that natural immunity from getting the flu was more powerful than any vaccine.
For some mysterious reason, these comments have gone by the wayside in recent years, as campaigns for yearly universal vaccination have intensified.
For some reason.
Republished from the author’s Substack
Join the conversation:


Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.









