In my part of the world, ‘Wrong Way Go Back’ is what the signs say if you try to drive onto the freeway down a slipway that is meant for cars coming off the freeway in the other direction.
The world is facing a similar scenario as governments prepare to fight the next pandemic with the methods that led to defeat in the Covid-19 pandemic.
Except that they all believe the opposite – they think it was a great triumph, that millions of lives (which only exist in a counterfactual virtual world) were saved, and that some minor improvements are needed that will lead to even better results next time.
And the vocal experts are telling them that the next time will be soon. We have hardly finished wrapping up the greatest pandemic (supposedly) in a hundred years and we are being warned that bird flu or ‘Disease X’ is just around the corner and we will have to do it all again.
Meanwhile, the evidence mounts that the Covid-19 response was at best ineffective, and at worst created many deaths that would otherwise not have happened. For whatever reasons, excess deaths continue to accumulate, at a lower rate in the countries that peaked earlier, which is the opposite of what we were led to expect.
We are told that there is a ‘scientific consensus’ that the methods used are effective and valid, but this cannot be true. Whether you agree with its ideas or not, the mere existence of the Great Barrington Declaration, originated by three of the world’s most highly qualified epidemiologists and signed by over 16,000 medical and public health scientists, is proof positive that there is no such consensus.
Governments around the world were hustled into adopting the one-size-fits-all strategy proposed by the notorious Imperial College London ‘Report 9’ – stopping the spread of SARS-CoV-2 by reducing the general level of activity in the population by 75%, as an interim measure until the development and deployment of an effective vaccine for all.
Governments deployed this ‘stopping the spread’ macro strategy at a point where there was no hard evidence of the effectiveness for the non-pharmaceutical interventions (NPIs) deployed. The state of scientific knowledge at the time did not support a consensus and it still does not. Comprehensive reviews of the use of NPIs in respiratory epidemics and pandemics prepared within the framework of evidence-based medicine in the years leading up to the Covid-19 epidemic (here and here) had concluded that there was only weak evidence in favour of them (for influenza).
Nothing has changed. There are a number of national reviews of the Covid-19 response at varying stages of progress. Only one of them has commissioned a similar evidence-based medicine review – the Scottish inquiry – and that review (by Dr Ashley Croft) came to the same conclusion, that there was only weak evidence that the measures had been effective.
While there are plenty of individual studies that purport to show that the measures were successful, each of them is dependent on carefully chosen parameters and assumptions that are open to evaluation and questioning. Different combinations yield different results. Bendavid and Patel get around this problem by choosing a ‘multiverse’ strategy: ‘Multiverse analyses elevate epistemic humility by relaxing the number of subjective choices in the research design process.’ They ran nearly 100,000 models based on possible variations in design parameters and found that:
…about half of all models suggest government responses were helpful, and half unhelpful when examining either of the three indices (stringency, government response, and economic support).
The upshot is that:
…we cannot conclude that there is compelling evidence to support the notion that government responses improved Covid-19 burden, and we cannot conclude that there is compelling evidence to support the notion that government responses worsened the Covid-19 burden.
Only hard and consistent evidence can justify extreme policies like confining a population to home detention and closing down most businesses.
But there are recurring problems we can observe with studies that seek to reinforce the macro strategy.
They often focus on the effect the chosen measure may have had on infections, and merely assume that reducing infections in a window of time will lead to better outcomes in terms of severe illness and mortality. These assumptions are unwarranted.
The time window is based on the difference between two points: one date when the NPIs are introduced, and another date some months further down the track. But this is vulnerable to the post hoc ergo propter hoc fallacy: the reduction in infections may have come about anyway without intervention. This is particularly the case with epidemics, which obviously follow an epidemic curve. If you choose your baseline date towards the top of the curve, a date, say, six months later will inevitably show fewer infections. You need to show that the intervention changed the course of the epidemic curve, that the actual level at the second date is lower than the expected level. This should be evident when graphed but is hardly ever done.
There are a number of levels at which the scientific record can be distorted to support a preconceived and biased policy position.
At the first level, decisions about what topics to research are biased by the availability of funding and by groupthink, as are the research findings that are then reported. Massive funding is available for patented pharmaceutical interventions, and a climate of opinion has been created in which these are favored strategies to counter a pandemic. Consequently, Big Pharma funded large-scale randomized-controlled trials (RCTs) for their vaccines. It is well known that trials funded by commercial interests are more likely to reach favourable findings, and many methodological failings have been revealed about the way these trials were conducted, for example by OpenVAET Josh Guetzkow et al, Peter Doshi et al. and as reported in TrialSiteNews.
At the second level, even when evidence for alternative treatments is available, it is ignored. For example, pre-Covid-19 there was already a systematic review in existence that showed that Vitamin D reduced the risk of getting a respiratory infection overall, and especially for those with a Vitamin D deficiency. But this was ignored. Since then, over 120 studies have nearly all shown that it significantly lowers the risk for mortality, hospitalization, and infection from Covid-19 specifically. Governments should have rolled vitamin D out to their populations, but they didn’t. They chose experimental, untried methods instead – there was no evidence whatsoever that confining whole populations to their homes would work.
A third line of defense is to design studies with parameters that favour your preferred intervention. Again, choose a slice of time in which the intervention worked, excluding the times when it didn’t work. With vaccines, Norman Fenton and Martin Neill have dubbed this ‘the cheap trick.’
A fourth line of defense is to reach conclusions that are not justified in the findings. If you cannot avoid publishing findings that you don’t like, include editorial commentary to undermine them. Thus, any papers that include findings unfavourable to Covid-19 vaccines will include a standard paragraph to the effect that despite these findings, the vaccines have been found to greatly reduce hospitalization and death [although they have never been found to reduce all-cause mortality] so that any contrary finding can safely be ignored.
The fifth line of defense is to craft a systematic review of the evidence so that it supports your favored position. A crucial strategy here is to invent selection criteria that will screen out the unfavourable research – or you can simply misrepresent the research that is included.
For example, take universal mask mandates. A recent systematic review of Masks and respirators for prevention of respiratory infections by Greenhalgh et al. (including some of the leading orthodox voices from my part of the world) makes a good case study. The review was designed to be a rejoinder to the Cochrane review of physical interventions, which concluded that: ‘Wearing masks in the community probably makes little or no difference to the outcome of influenza‐like illness (ILI)/Covid‐19 like illness compared to not wearing masks.’
Greenhalgh et al. criticize previous studies for combining dissimilar outcomes or settings – and then go on and do precisely the same. The forest plot summarizing their results for medical masks vs no masks is inconclusive, showing a diversity of outcomes on either side of the line, with no clear trend, consistent with the findings by Bendavid and Patel.
It would have been clearly negative overall if they had represented the results of the DANMASK study correctly. The numbers from that study that they include in their table for Figure 3 are not the results of the study as a whole but represent a sub-group, secondary outcome analysis of 9 infections in individuals wearing masks versus 16 with no masks. Apart from having very low numbers, this sub-group counted both respiratory and non-respiratory infections – apparently wearing masks protects you from gastroenteritis!
The overall ‘inconclusive’ conclusion of the DANMASK study was based on the whole study population of 4,862 and found that the difference between the mask wearers and the non-mask wearers was 42 to 53: ‘The between-group difference was -0.3 percentage point,’ and not statistically significant. And the study was not designed to show whether there were any improvements in severe illness or mortality, which remains unknown.
One of the other key studies included in the Greenhalgh review (by Suess et al.) was based on transmission within a household, not in the general population.
On these shaky foundations, the authors conclude that ‘masks work.’ But the data they review does not support the scenario they appear to recommend and that has generated controversy: general mandates for the entire population, whether infected or not or whether in contact with known infected individuals or not, to wear masks all the time while outdoors. They think they have shown that ‘masking is an effective (though not perfect) intervention for controlling the spread of respiratory infections’, but they have not.
Great pressure was brought to bear on the Cochrane Collaboration to change the conclusions of their review. The authors have stood firm and the findings have not been altered.
But the ‘scientific consensus’ will be represented as ‘masks work,’ even though the scientific record does not show this. The truth is that ‘the scientific consensus’ is based on opinion, not on the whole scientific record, and based on the opinions of orthodox scientists only, which in this case are hotly contested. Evidence that does not easily fit with dominant opinions is disregarded, either by completely ignoring its existence, or by editorial commentary. This is confirmation bias, which has been rampant in mainstream science and therefore in mainstream media.
By contrast, there is no equivalent of the Great Barrington Declaration for the laws of thermodynamics, which are not contested. There can be no scientific consensus about issues that are contested and are still under debate. Governments were sold a premature consensus of the orthodox.
Articles by orthodox experts often use the formulation ‘We now know.’ ‘We now know’ that masks work, and ‘we now know’ that NPIs in general are effective for controlling the spread of respiratory infections, whereas the scientific record shows a great diversity of findings and a great diversity of quality.
These orthodox experts are engaging in what would be called ‘apologetics’ in theology. Revealed truth cannot be contested, but apologetics is the search for the best rational arguments that will support the revealed truth.
The fundamental assumption on which the whole macro strategy was built is that governments should strive to manage or end a pandemic by stopping the spread. If this assumption cannot be substantiated, the macro strategy falls to the ground, and it cannot. A natural experiment took place in the slums of Mumbai. Commentators assumed that the mortality rate in these slums would be very severe because of the impossibility of ‘social distancing’ in crowded slums.
The actual outcome was the reverse, according to the empirical data presented by Malan et al. While the infection rate was higher in the slums (at the time of seroprevalence measurement in July 2020, 54 percent of the population compared with 15.1 percent elsewhere in Mumbai), the infection fatality rate was lower, only 0.076 percent as compared with 0.263 percent elsewhere. The implications of this finding are profound. The slum-dwellers benefited from a faster rate of infection. Not only that, but they also benefited from not being ‘socially distanced.’ This destroys the case for the macro strategy.
Elsewhere, the virus continued to spread, more slowly. In the US, nearly 60% of adults had been infected by May 2022, according to the CDC’s nationwide commercial laboratory surveillance system. And mortality continued to rise.
Many theories have been advanced by contrarians about how the management of the Covid-19 pandemic became a public health disaster, and why people have such diametrically opposed views about it, to the extent that we no longer have a common view of reality on these matters.
One explanation is that it was an episode of mass hysteria driven by fear, as proposed by Bagus et al (2021) or mass formation, as proposed by Mattias Desmet. This was fanned by an exponential surge in media coverage, reminiscent of the epidemic curve. Coverage of virus-related topics increased 55-fold by April 2020, according to Ng and Tan. Huang and Chen found that a quarter of all reporting in 2020 covered Covid-19. The pandemic became a global collective obsession.
One key factor in the derailing of the rational public health principles advocated by Reddy has been the complete policy failure to draw sound lessons even from the science that does get done, and to allow for the fact that the playing field is tilted by commercial interests to favour some policy positions over others.
Policy-making is dominated by a naïve realism (amounting to scientism) – if some scientists recommend something, no government can stand against them, because they are seen to be putting forward objective reality. Statistical figures in a table are accepted at face value, without any probing into the process by which they were calculated, which involves decisions and choices that can be questioned, and the conclusions derived from them can also be questioned. This could be termed an apparent objectivity fallacy. Orthodox scientists think they are in a simplistic war between science and anti-science, but not all science, and not all interpretations of the scientific record, are of equal value in guiding policy.
The science is dumbed down so that it can be given to the politicians, who decree standard operating procedures on a one-size-fits-all basis, and governments then use public relations techniques to reduce this further to sound bites that can be sold to the voters. In my state of Victoria, there were vox pops in the media (effectively qualitative exit polls) in the election immediately following the collapse of the Covid zero strategy, with voters telling reporters that they had voted for the government which had ‘kept them safe’ during the pandemic.
The Victorian State Government had ‘kept them safe’ by instituting the world’s longest lockdown in pursuit of Covid zero, which was never attainable. The government had closed the borders, confined the entire population to home detention, and closed most businesses for months on end. Australia’s outcomes, after four years, are similar to comparable countries.
In a remote island nation, we are used to strict border controls to keep out animal and plant pathogens. Keeping out human-borne pathogens is at least more feasible in countries you can drive to (with your pathogens), and so Australia, New Zealand, Iceland, and Japan were able to keep excess mortality down somewhat compared to countries like Italy and the poorer countries of Eastern Europe, but only in 2020. Geography (including human geography) matters – the poorer continental countries with mainly European populations were the worst affected. However, Covid zero was impossible – even for islands.
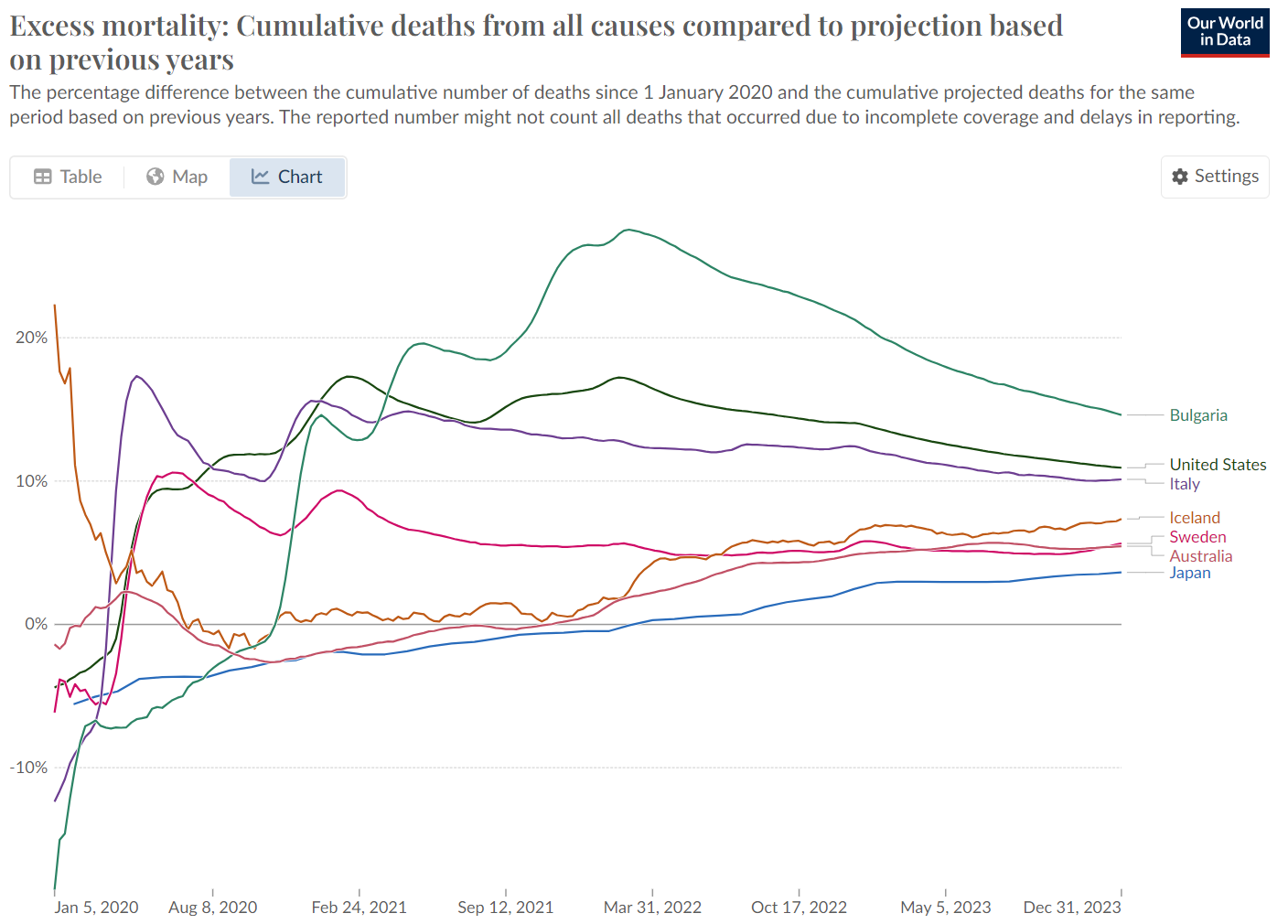
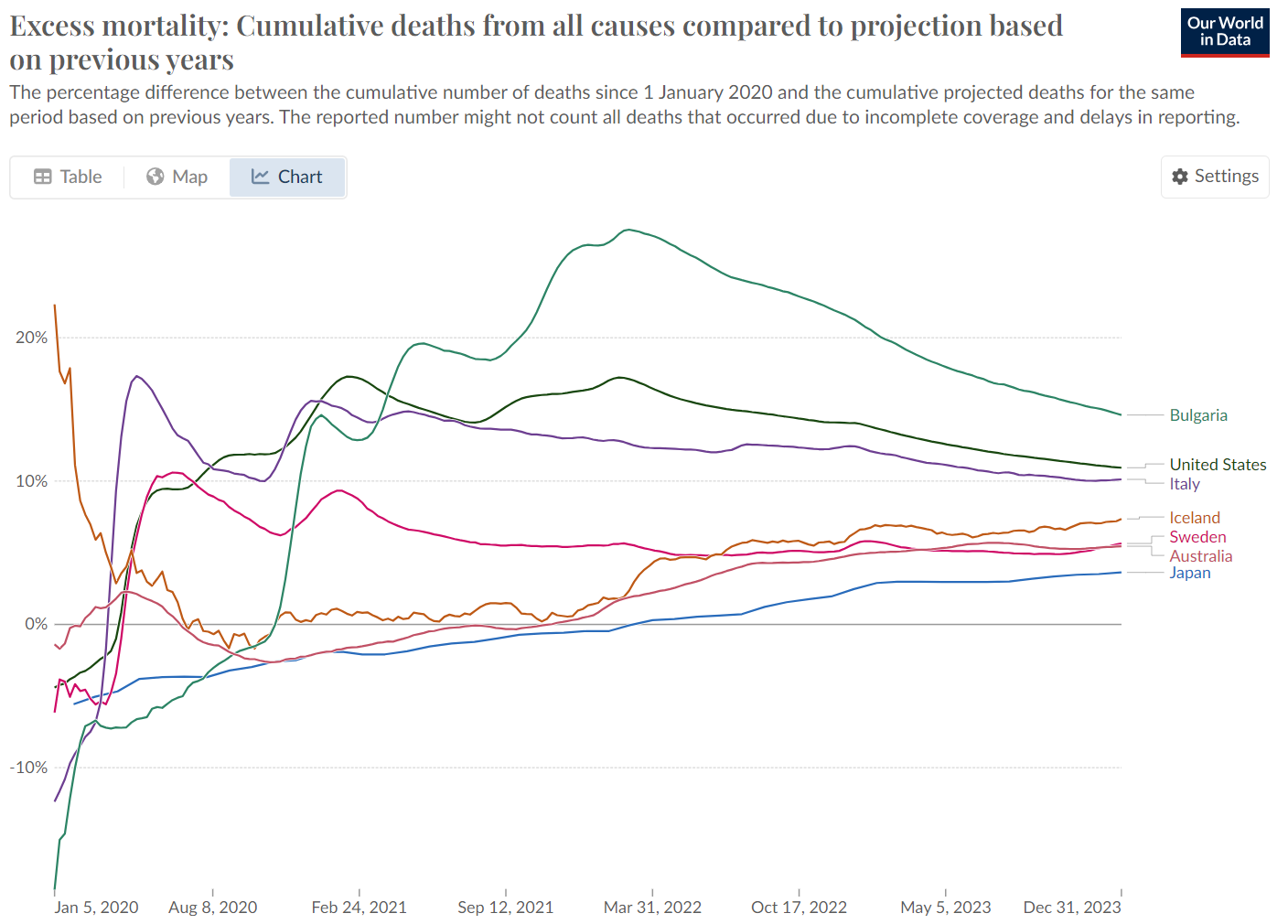
Governments did not stop the rapid spread of Covid-19 across most regions of the world, and universal vaccination did not end the pandemic or end the accumulation of excess deaths. Australian commentators pilloried Sweden for its more moderate approach and crowed about our better ‘performance,’ but after four years, Sweden had one of the lowest mortality totals in its region and was in a dead heat with Australia. Local commentators have gone strangely quiet about this.
Contemporary governments have powerful techniques at their disposal, starting with propaganda which is deployed to dominate the public ‘debate.’ A massive array of ever-changing bureaucratic rules was deployed to regulate everyday life, including when you could visit cafes, friends, and family, how long you could exercise outdoors and even to infringe on bodily autonomy, the last refuge against government. Australians like to think of themselves as rugged individualists, but almost everyone buckled down and obeyed the rules, rules that were grounded in contestable interpretations of the science. How could this happen?
We have to remember that we no longer (in Australia) live on remote farms in the outback, wrestling cattle. Across the globe, most of us live in highly regulated societies, with multiple tiers of overlapping government legislation and regulation. Even if we work in the private sector, private companies also confine us within a framework of bureaucratic rules and processes (such as standard operating procedures) which leave little room for individual initiative. Across the world, most people live within nested bureaucratic structures and are used to obeying the rules, however insane they might be. We are all too compliant.
And this is carried over into healthcare, which is essentially coercive at the best of times. Pharmaceutical chemicals coerce bodily functions for a few hours at a time and are incapable of healing, of building our health. That’s why we need to take the blue pills three times a day for years on end – because we don’t get better. And we go along with this too. Because science.
An underlying factor is that we are living through a great period of technological innovation, which has brought many benefits. But it brings with it a bias towards high-tech solutions, although there is no reason to believe these are necessarily more effective than low-tech solutions. Scientists are proficient at the technical level of analysis, but neither they nor their governments are proficient at the strategic level. Without sufficient skepticism and critical inquiry, biased technical conclusions drive biased strategies, and scientists become advocates, and then activists. Led by the WHO, the world is adopting standard operating procedures for ‘pandemic preparedness’ that divert resources away from the real challenges towards further futile attempts to ‘prevent’ future pandemics.
There is an important role for generalists in policy analysts in compensating for special interests and perspectives. Non-specialist policymakers need to be on their guard. Scientific conclusions can be fabricated, and government policy advisors need to run their own checks on what they are being told, looking for non-sequiturs, rhetorical manipulation, and cheap tricks. The way the system should work is that specialists make out their best case to non-specialists, who listen to a diversity of specialist views (much as in a courtroom) and then use critical inquiry to assemble the most sound opinion and evidence into a policy.
But they need the intellectual skills to do this, which they are not getting from universities, I am pained to report. Critical inquiry is supposed to be one of the most fundamental features of higher education and is usually prescribed in higher education standards across the world. In 2020, the world faced a fateful choice between two macro strategies. I am not aware of any medical faculty in the world where this strategic choice was debated either then or since, which is a serious indictment of a sector that should have been leading the scientific debate.
Students are simply not taught how to critique the leading assumptions of their discipline, or academic papers that support conventional thinking. Medical students are taught how to understand ‘the science’ not to critique it. Skepticism should be part of their regular approach, but in medicine, the name of skepticism is given only to those who defend orthodoxy by critiquing alternative schools of medicine. Instead of pointing out that the emperor has no clothes, they triumphantly proclaim that the beggar has no clothes!
I stand by my contention in a previous article that: ‘We need to revive the tradition of collegial debate and return to a dialectical and pluralistic model of knowledge.’ Instead, the correct interpretation of the ‘science’ is decided in closed committees and proclaimed by decree.
Governments are not being given good advice about public health and ‘pandemic preparedness’ and are being ‘blinded by science.’ It starts with the very definition of the problem and with the macro strategy that was advocated, snapped up, and implemented within weeks in February 2020. I can see no hard evidence that it is possible, or desirable, to ‘stop the spread’ of a respiratory pandemic over the medium term, as opposed to the unrepresentative slices of time in research studies. Covid-19 swept across the globe despite all attempts to stop it. And we have no empirical evidence that attempting to stop it lowered all-cause mortality over the period 2020-2022. Modelling is not evidence.
Large numbers of people with positive SARS-CoV-2 tests died in that time. But only a small proportion of them did not have the famous ‘comorbidities,’ only 6% according to the CDC in 2021. This tells us that it was in fact the comorbidities that were the problem. Too many of our elderly are living with poorly controlled hypertension, obesity, diabetes, heart disease, etc. A moderately unusual virus came along and pushed many of them over the edge. But this would not have happened if they had been in more resilient good health in the first place.
Building that resilience is an important goal for public health but has been overshadowed by pandemania.
Join the conversation:


Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.









