Many peer-reviewed research articles conclusively demonstrate that a low level of 25-hydroxyvitamin D in the bloodstream significantly increases the risk of severe disease, long-term damage, and death from COVID-19. That this information remains relatively unknown three years after the onset of the pandemic can be attributed to a pervasive pattern of corruption and/or glaring incompetence among many doctors, immunologists, public health officials, and mainstream media outlets.
In this article, we highlight research into the immune system’s dependence on the three “vitamin D” compounds: vitamin D3 cholecalciferol, 25-hydroxyvitamin D calcifediol and 1,25-dihydroxyvitamin D calcitriol. Only the first is a vitamin and all three molecules have very different roles. Only calcitriol can function as a hormone, but the immune system does not use hormonal signaling.
“Vitamin D” blood tests measure the level (concentration) of 25-hydroxyvitamin D in the bloodstream, because both the kidneys and the immune system rely on this as a supply for their signaling functions, which involve hydroxylating it to 1,25-dihydroxyvitamin D. 25-hydroxyvitamin D is made primarily in the liver, from vitamin D3 which is either ingested or is produced by the action of short-wavelength, high energy, ultraviolet B radiation on the skin.
In most populations, average 25-hydroxyvitamin D levels are half or less than the 50 ng/mL (125 nmol/L) required for optimal immune system function. Additionally, we explain the 25-hydroxyvitamin D-based intracrine and paracrine signaling systems which many types of immune cells rely on to respond to their changing circumstances. Furthermore, we present a vitamin D supplementation protocol that reliably attains at least 50 ng/mL of 25-hydroxyvitamin D over several months, along with methods for achieving this level in clinical emergencies within approximately four days or even four hours.
There is very little vitamin D3 in food. UV-B radiation is difficult to obtain except on cloudless days with high elevation sunlight – and it always damages DNA and so raises the risk of skin cancer.
Good health can only be obtained with at least 50 ng/mL circulating 25-hydroxyvitamin D. This is the only way of ensuring that SARS-CoV-2 and influenza do not spread in pandemic fashion and do not seriously harm and kill many of those who are infected. Sepsis, which kills around 11 million people a year worldwide, would be rare if everyone had at least 50 ng/mL circulating 25-hydroxyvitamin D.
Fortunately, very small quantities of vitamin D3 are required – and it is safe, inexpensive and well-researched.
We also discuss the excessive, indiscriminate cell destroying, inflammatory immune responses which are the cause of most of the harm and death from COVID-19 and which cause numerous other acute and chronic illnesses, especially sepsis. Inadequate 25-hydroxyvitamin D makes these responses much worse, but their fundamental cause is an evolutionary adaptation to helminths (intestinal worms) which is exposed now that we are no longer infested with these multicellular parasites.
Vulnerable Populations and Vitamin D Deficiency
Elderly individuals, those with dark or black skin living far from the equator, and people who avoid exposure to ultraviolet B light typically have even lower levels of 25-hydroxyvitamin D than those who are younger, with less pigmented skin, who live closer to the equator or who expose more bare skin to direct sunlight.
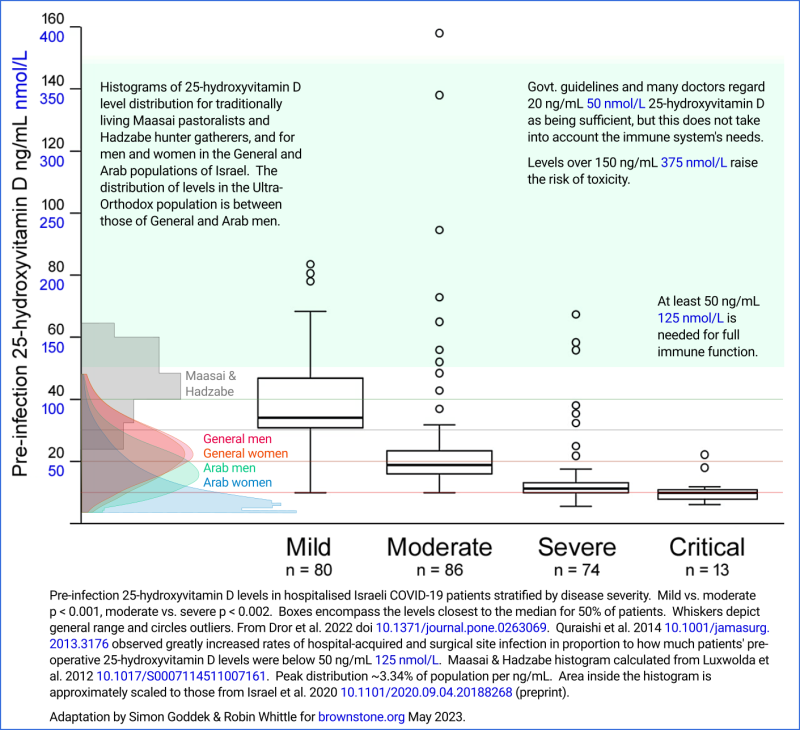
Low levels of 25-hydroxyvitamin D in the bloodstream are the primary risk factor for severe COVID-19 cases and fatalities. While advanced age and obesity are recognized risk factors, these conditions contribute to even lower levels of 25-hydroxyvitamin D compared to younger and non-obese individuals. In 2022, Dror et al. conducted a study titled “Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness,” which clearly demonstrated the link between 25-hydroxyvitamin D levels and COVID-19 severity. The study analyzed 25-hydroxyvitamin D levels in the bloodstream of 253 COVID-19 patients hospitalized in northern Israel between April 7, 2020, and February 4, 2021, prior to their infection. The results were presented using box and whiskers plots for mild, moderate, severe, and critical cases, as depicted in the graph above.
Dror et al. found that patients with “vitamin D deficiency” (<20 ng/mL 25-hydroxyvitamin D) were 14 times more likely to experience severe or critical disease than patients with levels of ≥40 ng/mL (odds ratio [OR], 14; 95% confidence interval [CI], 4 to 51; p < 0.001).
Due to statistical uncertainties, the actual rate at which severe or critical disease is associated with <20 ng/mL vs. ≥40 ng/mL 25-hydroxyvitamin D levels in the sampled population is known with 95% confidence to be between 4 and 51. The statistical significance of this observation is “p < 0.001”. This means that if there was no relationship between pre-infection 25-hydroxyvitamin D levels and disease severity, it would take more than 1000 trials like this one, on average, before sampling error would result in a deviation as strong as the current observations.
These results should have been celebrated globally, as they show that maintaining adequate vitamin D3 levels of at least 40 nanograms per milliliter is a simpler, safer, less costly and more effective approach to mitigating COVID-19 severity and death than vaccines, lockdowns, social distancing, and masks.
It is relatively simple to comprehend the significance of proper vitamin D3 supplementation for immune system health, and consequently for COVID-19, sepsis, influenza, and many other diseases. The reasons why a majority of doctors and immunologists exhibit limited interest in vitamin D, and thus remain unaware of its importance, are far more intricate and perplexing.
Vitamin D3, 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D
Here, we briefly explain the importance of the three primary vitamin D compounds to the immune system in general, and to COVID-19 in particular, correcting errors and filling gaps in the most common patterns of (mis)understanding these compounds. A more extensive, illustrated tutorial can be found at: vitamindstopscovid.info/00-evi/.
There are very limited amounts of vitamin D3 (cholecalciferol) in foods, whether fortified or not. Food sources alone are inadequate for human health. Substantial quantities of vitamin D3 can be produced in our skin when ~297-nanometer wavelength ultraviolet B (UV-B) radiation breaks a carbon ring in 7-dehydrocholesterol, and the resultant molecule reconfigures itself to become vitamin D3 cholecalciferol. This UV-B is at the very high frequency, high energy, short wavelength extremity of the Sun’s spectrum. It is only available naturally from high-elevation sunlight on cloud-free days, without passing through glass, clothing, or sunscreen. While there are many healthful aspects of sunlight exposure, UV-B always damages DNA and thus raises the risk of skin cancer. This makes UV-B skin exposure impractical for supplying the vitamin D3 the body needs – and those with dark or black skin would need hours of strong exposure per day to generate the vitamin D3 they need.
Fortunately, supplemental vitamin D3 is safe and effective for maintaining the 50 ng/mL or greater 25-hydroxyvitamin D levels the immune system needs to function properly. For 70 kg (154 lb) body weight without obesity, 0.125 milligrams a day will attain this level after several months. This is also known as “5,000 International Units” per day. This equates to a gram every 22 years – and pharmaceutical grade vitamin D3 costs about USD $2.50 per gram, ex-factory.
If most people, or everyone, achieved at least 50 ng/mL 25-hydroxyvitamin D, such as by supplementing vitamin D3 sufficiently, there would be no pandemic influenza or COVID-19, because most people’s immune systems would work properly, in contrast to their limited performance today. Those who were infected would only rarely suffer serious harm or be killed. Human health would be improved in numerous other ways in a revolution at least as significant as those which brought us sanitation and antibiotics.
Common responses to these claims are that vitamin D is just another over-hyped nutrient and that if vitamin D was indeed so important, most doctors would already recognise this. The research is very clear, but not widely understood.
Vitamin D2 (ergocalciferol) is a similar molecule to vitamin D3 (cholecalciferol). Its 25-hydroxy and 1,25-dihydroxy derivatives function similarly to those of vitamin D3 but are somewhat less effective. Here, we focus on the three naturally occurring compounds:
- Vitamin D3 cholecalciferol: Ingested or produced in the skin by the action of UV-B light.
- 25-hydroxyvitamin D calcifediol (also known as calcidiol): Produced from vitamin D3, primarily in the liver.
- 1,25-dihydroxyvitamin D calcitriol: This compound binds to and activates the “vitamin D receptor” molecule, which would be better known as the “calcitriol receptor.” These activated receptors profoundly change the cell’s behavior by up- and down-regulating the transcription of dozens or hundreds of genes to mRNA molecules, which in turn tell the cell’s ribosomes which proteins to make. The pattern of which genes are up- and down-regulated varies from one cell type to another.
The latter two compounds are the vitamin D3 molecule with oxygen-hydrogen hydroxy groups bonded to its 25th carbon and to its 1st and 25th carbon, respectively. Their proper names include “D3” but the names are long enough already and the “3” is often omitted.
Vitamin D3 circulates in the bloodstream and has, at best, only a minor direct impact on the immune system. Over a week or so, it is processed, mainly by the liver, so that about 1/4 of it is hydroxylated to 25-hydroxyvitamin D, which circulates in the bloodstream. The rest is degraded and/or excreted. 25-hydroxyvitamin D has a relatively long half-life: a month or so for lower levels and weeks for healthy and higher levels.
Neither vitamin D3 nor 25-hydroxyvitamin D function as hormones. A hormone is a long-distance signaling molecule whose level in the bloodstream is controlled by one part of the body. The level (concentration) of the hormone in the bloodstream is detected by one or more cell types anywhere else in the body, including in the brain and spinal cord, in ways that affect those cells’ behavior. The immune system does not use hormonal (endocrine) signaling.
All doctors understand that 1,25-dihydroxyvitamin D calcitriol can function as a hormone. The parathyroid gland senses the level of circulating calcium and signals this to the kidneys via the parathyroid hormone. This controls the extent to which the kidneys hydroxylate 25-hydroxyvitamin D to form a tightly controlled, very low level of circulating 1,25-dihydroxyvitamin D. This has a half-life of less than a day, and its level hormonally controls several crucial aspects of calcium-phosphate-bone metabolism by affecting the behavior of multiple cell types in the intestine, kidneys, and bone. While vitamin D’s role in the immune system is increasingly appreciated, most doctors – and many vitamin D researchers – mistakenly assume that the immune system is somehow hormonally “regulated” by the kidney’s very low level of circulating 1,25-dihydroxyvitamin D.
Despite Reinhold Vieth’s 2004 warning, the field remains plagued to this day by two common terminological and conceptual errors:
- While “vitamin D” is an appropriate collective term for the three compounds, many researchers use it to refer to just one compound, as if all three were much the same, when they should specifically identify the compound itself.
- This gives rise to the conflation of 1,25-dihydroxyvitamin D calcitriol, which can act as a hormone, as being just one form of vitamin D and therefore being much the same as vitamin D3. This leads to the common falsehood that “vitamin D is a hormone.” This misconception scares many people away from properly supplementing vitamin D3, especially when the required daily quantity is expressed as thousands of impressive-sounding International Units. 1,25-dihydroxyvitamin D calcitriol is not a vitamin, and its role is a completely different compound from that of vitamin D3 cholecalciferol, just as 25-hydroxyvitamin D’s role differs entirely from the roles of the other two.
Having outlined the long-established, kidney-centric understanding of the three vitamin D compounds, we now turn to the more recently discovered and still only rarely understood importance of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D to the immune system.
Understanding Immune Cell Signaling and the Role of 25-Hydroxyvitamin D
Many types of immune cells rely on a suitably high level of 25-hydroxyvitamin D in the bloodstream in order for these molecules to diffuse into each cell’s cytosol (the fluid in the main body of the cell) in sufficient quantities to support these cells’ intracrine and paracrine signaling systems.
Intracrine signaling occurs entirely within a single cell. The cell detects a specific external condition, such as through receptor molecules that span its membrane and identify the presence of particular molecules outside the cell. This detection prompts the cell to produce, internally, a small but significant quantity of a signaling molecule, which functions as an intracrine agent, by activating a receptor molecule inside the same cell. These activated receptor molecules alter gene transcription, subsequently changing protein synthesis and causing the cell to change its behavior in response to the external condition it detected.
Autocrine signaling is similar, except that the internally generated autocrine agent activates receptors on the outside of the same cell. It is a common mistake to confuse intracrine and autocrine signaling.
Paracrine signaling may coexist with intracrine or autocrine signaling. The signaling molecule, produced by a cell in response to particular circumstances, diffuses out of the cell in which it was made, raising the level of this compound in the local area, where it functions as a paracrine agent to alter the behavior of other nearby cells, usually of different types.
25-hydroxyvitamin D-based intracrine signaling is essential for the ability of many types of immune cells to respond to each cell’s changing circumstances. This was elucidated in the late 2000s by Martin Hewison and colleagues in the UK, working with macrophages and dendritic cells.
The third kind of immune cell in which 25-hydroxyvitamin D-based intracrine signaling has been studied is Th1 regulatory lymphocytes from the lungs of hospitalized COVID-19 patients. This is the beautiful work of a large team of investigators, Chauss et al. 2021 in Nature Immunology: Autocrine vitamin D signaling switches off pro-inflammatory programs of Th1 cells.
Many other types of cells, particularly those of the immune system that are not involved in calcium-phosphate-bone metabolism, are known to change their gene expression significantly in response to their vitamin D receptor molecules being activated by binding to 1,25-dihydroxyvitamin D calcitriol. It is reasonable to assume that all these types of cell also utilize 25-hydroxyvitamin D-based intracrine and/or paracrine signaling.
The levels of intracellular 1,25-hydroxyvitamin D produced when the intracrine signaling system is activated are considerably higher than the very low, hormonal level of extracellular 1,25-dihydroxyvitamin D, which is approximately 0.12 ng/mL. Therefore, this hormonal 1,25-dihydroxyvitamin D has no significant effect on immune cells or the entire immune system.
These cells can only respond to their changing circumstances fully and rapidly if sufficient 25-hydroxyvitamin D diffuses into their interior to supply and maintain its conversion to 1,25-hydroxyvitamin D (which has a very short half-life) when the cell’s intracrine signaling system is activated by whatever external condition that cell type detects.
The need for at least 50 ng/mL (125 nmol/L) circulating 25-hydroxyvitamin D
Intracellular 25-hydroxyvitamin D levels cannot be measured. No cell-biology research to date has demonstrated that at least 50 ng/mL of circulating 25-hydroxyvitamin D is required to supply this compound – which is a raw material, not a signaling molecule – to cells in sufficient quantities for each cell to be able to rapidly and fully perform its intracrine signaling conversion to 1,25-dihydroxyvitamin D. However, we can infer this from the increasing degree of immune system dysfunction that occurs the further the circulating 25-hydroxyvitamin D level is below 50 ng/mL – which is one part in 20,000,000 by mass. This relation is evident in many diseases, and the decline of health with lower 25-hydroxyvitamin D levels is clearly evident in Dror et al.’s observations, depicted above.
The kidneys can generally produce sufficient hormonal 1,25-dihydroxyvitamin D with 20 ng/mL or more circulating 25-hydroxyvitamin D. In developed countries, government vitamin D supplementation guidelines aim to attain this 20 ng/mL level without regard to the needs of the immune system. (Kimball and Holick 2019.)
In 2008, 48 leading vitamin D researchers called for the standard of vitamin D repletion to be 40 to 60 ng/mL of circulating 25-hydroxyvitamin D. Since the early 2000s, these and other researchers have been arguing with government guideline committees about the need for vitamin D3 supplementation in quantities that attain such levels.
The 2011 Endocrine Society recommendation has a target of 40 ng/mL to ensure virtually all individuals have a level above 30 ng/mL. Toxicity, in the form of excessive calcium levels and bone mineral density loss can occur but 25-hydroxyvitamin D levels “need to be above 150 ng/mL before there is any concern”. From this they derive, rather arbitrarily, a “safety margin” upper limit of 100 ng/mL.
These researchers’ ~50 ng/mL target has been vindicated by a large body of research, one strong example being the 2014 research of doctors in a Boston hospital on the risk of both hospital-acquired and surgical site infections, as a function of pre-operative 25-hydroxyvitamin D levels: Association Between Preoperative 25-Hydroxyvitamin D Level and Hospital-Acquired Infections Following Roux-en-Y Gastric Bypass Surgery.
The subjects were 770 morbidly obese patients who underwent the same gastric bypass weight loss surgery. Obesity reduces the ability of the body to convert vitamin D3 into circulating 25-hydroxyvitamin D, but there is no reason to believe that it alters the level of circulating 25-hydroxyvitamin D which immune cells require to properly run their intracrine and paracrine signaling systems. So these Boston observations are applicable to all people.
What they found was striking. Their graphs (below combined into one) are easily understood and should be displayed in doctors’ offices and waiting rooms because they are so pertinent to all aspects of health.
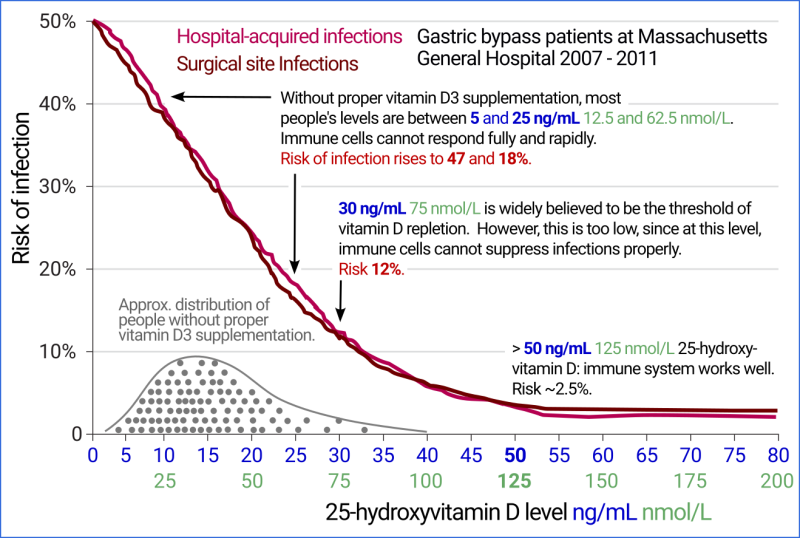
For those patients with 50 ng/mL or more circulating 25-hydroxyvitamin D (which would have been attained largely or entirely by proper vitamin D supplementation), the risk of hospital acquired and surgical site infections, separately, were about 2.5%. 20 ng/mL is a perfectly ordinary level for someone who does not supplement vitamin D3 much or at all and who has not recently had extensive UV-B skin exposure (or who has, but on dark or black skin). The Boston hospital research shows that such people have a 24% chance of each type of infection.
This tremendous increase in infections is due to weakened innate and adaptive responses to the bacteria which are the primary cause of both types of infection. Some degree of confounding may exist in these Boston hospital results, such as people who are generally healthier happening to take more vitamin D3 without this affecting their ability to defend against bacterial infections. However, the relationship is clear and strong and the intracrine and paracrine signaling mechanisms are now so well understood that it is reasonable to assume confounders are only responsible for a small fraction of this relationship, and that the great majority of it is due to low 25-hydroxyvitamin D levels causing immune dysfunction.
We can see from the histogram of 25-hydroxyvitamin D levels in the graph at the start of this article (from Israel et al. 2020) that even in sunny Israel, a significant fraction of the population – especially Arab women – have 25-hydroxyvitamin D levels in the 5 to 10 ng/mL range, 1/10th to 1/5th of what their immune system needs. At 5 ng/mL, the Boston hospital risk for both hospital-acquired and surgical site infections rises to 47%.
In the histogram for Arab women, the lowest bar, for 4 to 5 ng/mL, is much higher than the trend line. This is because some of these women had levels below the 4 ng/mL detection limit. These terribly low levels result, in large part, from these women’s clothing covering most of their body, and their sun avoidant lifestyles.
This combination of observations and mechanistic understanding makes it very clear that most people, in most countries, for most or all of their lives, have insufficient 25-hydroxyvitamin D to run their innate and adaptive immune responses to bacterial pathogens. The same intracrine and paracrine signaling systems are also reasonably assumed to be just as crucial for the immune system’s ability to mount strong innate and adaptive responses to cancer cells, fungi, and viruses.
This article has veered from a discussion of COVID-19 into a crash tutorial on 25-hydroxyvitamin D-based innate and adaptive signaling. This is necessary in order to understand why good human health, including especially regarding COVID-19, can only be attained with at least 50 ng/mL circulating 25-hydroxyvitamin D. No amount of drugs, vaccines, lockdowns, masks, monoclonal antibodies, anti-viral drugs etc., can make up for the immune system being crippled, which it will be to a significant degree when 25-hydroxyvitamin D levels are below 40 ng/mL.
While there is a growing awareness of the importance of vitamin D for the immune system, few clinicians or researchers understand 25-hydroxyvitamin D-based intracrine and paracrine signaling. Many assume that the immune system is somehow regulated by the same hormonal 1,25-dihydroxyvitamin D that the kidneys use to control the behavior of distant cells, of multiple types, which are involved in calcium-phosphate-bone metabolism. This has led some clinicians to treat sepsis and COVID-19 by raising this level of circulating 1,25-dihydroxyvitamin D, both without success. As noted in the Front Line COVID-19 Critical Care Alliance (FLCCC) MATH+ hospital protocol, this calcitriol therapy has minimal effect on immune cells and can lead to toxicity by raising blood calcium levels excessively.
Far too many research articles state that “vitamin D regulates the immune system”. This leads many researchers and clinicians to assume that the hormonal model also applies to the immune system. In fact, none of the three vitamin D compounds regulate anything. The parathyroid and kidneys regulate calcium-phosphate-bone metabolism, with the kidneys using circulating 1,25-dihydroxyvitamin D as an endocrine agent (hormone) to control the behavior of distant cells for this purpose.
The immune system regulates itself with multiple interrelated mechanisms. A crucial part of this is the ability of individual cells to respond to their changing circumstances. Many types of immune cell, when they sense a particular cell-type specific condition, generate 1,25-dihydroxyvitamin D as an intracrine agent, entirely within the cell, to change that cell’s behavior. Some of this diffuses to nearby cells where it may act as a paracrine agent to alter their behavior. 1,25-dihydroxyvitamin D is a signaling molecule. Vitamin D3 and 25-hydroxyvitamin D are not. Vitamin D3’s role is to be converted into circulating 25-hydroxyvitamin D, which is needed by the kidneys, and – at a higher level – by multiple types of immune cell.
Dysregulated, indiscriminate, cell-destroying inflammatory responses
Low 25-hydroxyvitamin D levels weakening innate and adaptive immune responses explains a great deal of ill-health suffered by many people today. However, there is another aspect of the immune system that suffers potentially devastating effects when immune cells cannot get enough 25-hydroxyvitamin D: excessive inflammation. Here, we focus on excessive inflammation in the acute diseases COVID-19 and sepsis, rather than the chronic excessive inflammation which drives autoimmune diseases.
When COVID-19 severely harms or kills, it is the immune system that causes the debilitating and fatal damage, not the virus – which by then has stopped replicating. The FLCCC’s MATH+ protocol makes this clear:
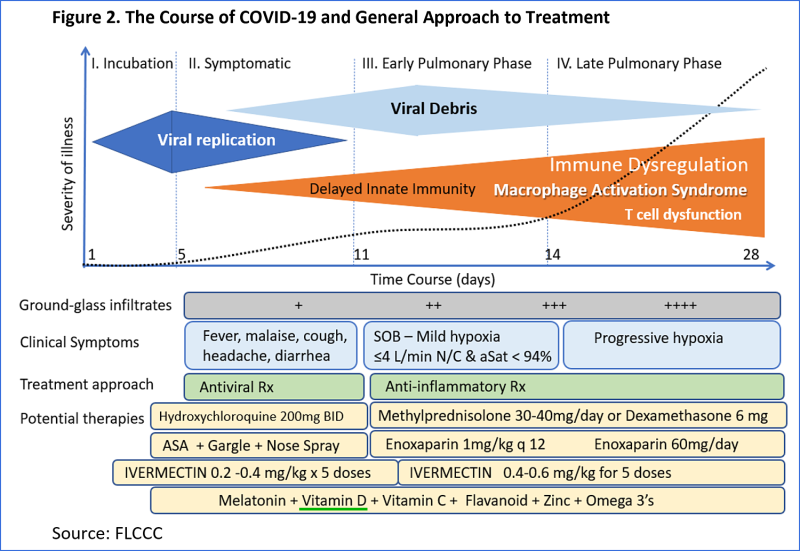
When symptoms are severe enough to warrant hospitalization, the battle is against the dysregulated hyper-inflammatory immune responses, not viral replication. Patients only reach this state if their innate and adaptive responses have failed to suppress the viral infection and the virus has become active in their lungs. The excessive inflammatory response to this infection results in the destruction of pulmonary endothelial cells – those lining the blood vessels of the lung. The body responds to this pervasive vascular damage by thickening the blood, so it is ready to plug the leaks. The hyper-coagulative blood forms micro-embolisms (clots) in the fine capillaries of the lungs in which oxygen and carbon dioxide are exchanged. This blocks circulation in entire sections of the lungs, exacerbating the reduced oxygenation caused by the fluid buildup (pneumonia) in the alveoli (tiny air sacs) where this exchange occurs.
The most common cause of death is hypoxia. Micro-embolisms and larger clots also block circulation and cause permanent, potentially fatal damage in all other organs, including the heart, brain, spinal cord, and liver.
The 2020 Th1 lymphocyte research which should have ended the pandemic
“T cell dysfunction” is mentioned in the MATH+ diagram, which brings us to Chauss et al. 2021, first published as a preprint in July 2020, in which the researchers studied Th1 regulatory lymphocytes retrieved from the lungs of hospitalized COVID-19 patients. For the first time, they elucidated this cell type’s reliance on 25-hydroxyvitamin D-based intracrine signaling. Th1 cells produce a pro- and an anti-inflammatory cytokine (short-range immune system signaling molecule). In their startup program, upon being activated in the lungs of these patients, each Th1 cell is pro-inflammatory: its production of the pro-inflammatory cytokine is greater than that of the anti-inflammatory one.
These lymphocytes detect a particular external condition (a high level of a complement protein), via receptors on their cell surface. This causes the cell to activate its 25-hydroxyvitamin D-based intracrine signaling system, by producing both vitamin D receptor (VDR) molecules in the body of the cell, and the 1-hydroxylase enzyme which converts 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D (calcitriol). Each of these molecules binds to a VDR molecule and so forms an activated VDR-1,25-dihydroxyvitamin D complex.
When this signaling system works properly, the activated complexes find their way to the nucleus and up- and down- regulate the transcription of hundreds of genes, which alters the cell’s protein production and so changes its behavior. The cell switches to its anti-inflammatory shut-down program: greater production of the anti-inflammatory cytokine than of the pro-inflammatory one.
This dense cell biology article describes the precise, molecular steps by which all this should occur. It also explains how this intracrine signaling system fails in the Th1 cells from the lungs of hospitalized COVID-19 patients. This means the Th1 cells continue to boost inflammatory responses in the lungs indefinitely. This – and likely similar failures of 25-hydroxyvitamin D intracrine and paracrine signaling in other types of immune cells – leads to excessive inflammation, endothelial cell damage, and subsequent harm and death resulting from pneumonia, hypoxia, and organ damage.
The same failure or weakening of 25-hydroxyvitamin D based intracrine signaling in other types of immune cell which directly protect against the viral infection is surely a crucial factor in the infection continuing for more than a few days and progressing to the lungs.
Chauss et al. found that the primary or sole reason for this failure was inadequate 25-hydroxyvitamin D in these Th1 lymphocytes. The researchers had no data on patients’ circulating 25-hydroxyvitamin D levels, but we know from research such as that of Dror et al. that COVID-19 patients in intensive care and those who die typically have even lower 25-hydroxyvitamin D levels than the general population – most of whom have only a fraction of what their immune systems need to function properly.
For each Th1 cell’s intracrine signaling system to function properly, 25-hydroxyvitamin D must diffuse from the bloodstream and across the cell’s plasma membrane into its cytosol (internal fluid) in a quantity sufficient to ensure that when the cell’s intracrine signaling system is activated, conversion to 1,25-dihydroxyvitamin D proceeds at the required rate, and that 25-hydroxyvitamin D continues to diffuse into the cell to replace those molecules just converted. Inadequate intracellular 25-hydroxyvitamin D means that the intracrine signaling system cannot produce sufficient 1,25-dihydroxyvitamin D to activate the number of VDR molecules required to properly alter the cell’s behavior.
All the above information has been available in research articles or preprints since mid to late 2020, before any mRNA and adenovirus vector vaccines were administered, and before the lockdowns and suppression of early treatment became so destructive. No use was made of this information by those who directed the mainstream pandemic response, and to this day, very few people – including doctors and immunologists – seem to understand it.
The primary reason for this ignorance is that the majority of immunologists and doctors are not interested in such research.
Doctors and immunologists are very busy. Their fields involve heavy responsibilities and the ideal of acquiring vast amounts of knowledge. Academic journals are awash with articles in general, especially regarding COVID-19.
However, if immunologists and doctors, as whole, global, professional groups which humanity completely rely upon, were diligently seeking out and raising awareness of the most important research, then Chauss et. al. would quickly have become widely known, even as a preprint. First, a handful of these professionals would have read it. Then they would have told their colleagues, who would also have recognized the decisive role this new knowledge could play in the pandemic response. They would have told others, word would have spread, the mainstream media would have written about it, and soon governments would be acting accordingly to protect the public by raising most people’s 25-hydroxyvitamin D levels. Hospitalized patients, healthcare workers, the elderly, the incarcerated and other vulnerable people would have been prioritized.
This response to the pandemic would have suppressed it by late 2020 or early 2021, without relying on vaccination, masks or lockdowns – especially if it was combined with a growing number of safe, inexpensive, highly effective early treatments, of which ivermectin is now the best known.
This collective lack of interest in the most important research, in a global crisis, constitutes an egregious level of ineptitude which was, and still is, compounded by pervasive corruption and by governments and corporations working together to suppress debate. Consequently, tens of millions have died when the whole pandemic could have been suppressed worldwide with proper vitamin D3 supplementation by the end of 2020. The WHO reported that approximately 14.9 million people had been killed by the pandemic in 2020 and 2021– directly by the illness and indirectly, such as by not being able to access hospital treatment for other conditions.
If doctors and immunologists – or even the mainstream media – had been properly interested in such important research, a proper understanding of vitamin D would have spread widely before the COVID-19 pandemic. For instance, regarding hospital-acquired infections, predating and confirming the findings in the 2014 Boston hospital research, Youseff et al. 2012 and Laviano et al. 2020, who observed a 48% increase in post-operative infections for every 10 ng/mL reduction in pre-operative 25-hydroxyvitamin D.
One of us (RW) wrote to the W.H.O. Strategic and Technical Advisory Group for Infectious Hazards (STAG-IH) on 2020-03-22 about vitamin D and other nutrients to tackle COVID-19.
Leading vitamin D researchers rushed to explain the need for good 25-hydroxyvitamin D levels to tackle the pandemic, though not in conventional peer-reviewed journals: Wimalawansa 2020-02-28 and Grant & Baggerly 2020-04-09.
A thoroughly referenced peer-reviewed article Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection Mansur et al. 2020-05-18 would have saved millions of lives if doctors and immunologists had paid it proper attention.
Attaining 50 ng/mL 25-hydroxyvitamin D
Food can provide only a small fraction of the vitamin D3 we need to maintain good health. UV-B skin exposure is neither a safe nor easily accessible method for generating most or all of the vitamin D3 our bodies require. Proper vitamin D3 supplementation is the only way for most people to achieve the 25-hydroxyvitamin D levels their immune systems need to function properly. The daily quantities are minimal; for convenience and cost reduction, larger doses can be taken every 7 to 10 days. Current government-approved vitamin D3 supplemental guidelines are insufficient. They aim to achieve a circulating 25-hydroxyvitamin D level of just 20 ng/mL, which is generally adequate only for kidney function and bone health. These guidelines typically specify supplemental amounts based on age group, often with a maximum daily intake of 0.1 to 0.25 mg (4,000 to 10,000 IU).
To achieve healthy 25-hydroxyvitamin D levels for all individuals, we cannot rely solely on these recommendations, blood tests, or medical monitoring. Fortunately, there is a relatively wide range of healthy vitamin D3 intakes for each person, owing to the self-limiting actions of enzymes that degrade 25-hydroxyvitamin D at a rate proportional to its level in the body. As a result, doubling the vitamin D3 intake is likely to increase 25-hydroxyvitamin D levels by only 40 to 50%.
In order to achieve healthy 25-hydroxyvitamin D levels of at least 50 ng/mL, and up to 90 or 100 ng/mL without medical monitoring, it is both necessary and sufficient to specify the average daily vitamin D3 supplemental intake as a ratio of body weight, or within a range of two ratios, with higher ratios for those suffering from obesity. Ideally, leading vitamin D researchers would already have written a consensus journal article to this effect. Recommendations consistent with this approach can be found in a 2022 Nutrients article by Emeritus Professor of Medicine Sunil Wimalawansa (University of Texas Medical Branch at Galveston and Robert Wood Johnson Medical School, New Jersey): “Rapidly Increasing Serum 25(OH)D Boosts the Immune System, against Infections – Sepsis and COVID-19.” These recommendations include the following ranges of ratios:
- Normal and overweight: 60 to 90 IU per kilogram body weight, per day. Thus, 0.125 mg (5,000 IU) daily, or a 50,000 IU capsule every 10 days, is suitable for individuals weighing 56 to 83 kg (122 to 183 lbs).
- Obesity I & II (BMI 30 to 39): 90 to 130 IU per kg body weight per day.
- Obesity III (BMI 40 or more) – a condition requiring medical attention: 140 to 180 IU per kg body weight per day.
Ratios of bodyweight for underweight, normal and overweight people, with higher ratios for those suffering from obesity, can be derived from Afshar et al. 2020 who found that 70 to 100 IU vitamin D3 a day per kg bodyweight, for over 500 neuro-opthamology patients since 2010, resulted in long-term 25-hydroxyvitamin D levels between 40 and 90 ng/mL. In general, those at the lower end of this range would have been suffering from obesity.
Ekwaru et al. 2014 analyzed long-term 25-hydroxyvitamin D levels according to daily supplemental intake quantities for four self-described body morphologies: underweight, normal, overweight and obesity. From this it is possible to conclude that in order to attain 50 ng/mL 25-hydroxyvitamin D, those suffering from obesity needed approximately 43% more vitamin D per day, as a ratio of bodyweight, than those not so suffering.
Prof. Wimalawansa adapted this derivation to the ranges of ratios just mentioned, which we summarize in a simplified manner in the following table:
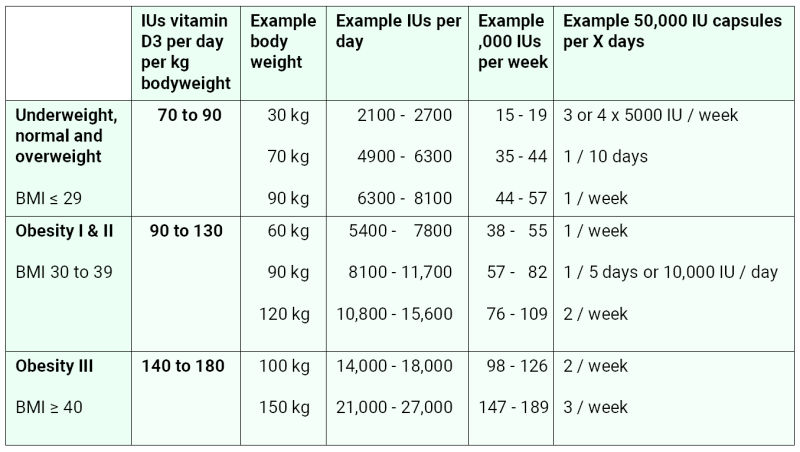
He also recommended 70 IU vitamin D3 / kg BW / day for age 18 years and younger (with no correction for obesity) and lower ratios for underweight adults.
Research indicates that two mechanisms cause people suffering from obesity to attain lower 25-hydroxyvitamin D levels than those without obesity, for any given ratio of vitamin D3 supplemental intake and body weight: reduced hydroxylation of vitamin D3 in the liver and increased absorption of 25-hydroxyvitamin D in excess adipose tissue. These mechanisms are specific to obesity. We know of no mechanistic or observational evidence for lower ratios for underweight people.
By following body weight ratio based recommendations such as those made by Prof. Wimalawansa, people of all ages, weights and body morphologies will attain at least 50 ng/mL of circulating 25-hydroxyvitamin D over several months, with levels rarely exceeding 100 ng/mL, without the need for blood tests or medical supervision.
Rapidly raising 25-hydroxyvitamin D levels in clinical emergencies
Although 5,000 IU may seem like a substantial amount of vitamin D3, this minuscule 1/8000th of a gram does little in a single day to elevate unsupplemented average 25-hydroxyvitamin D levels, which typically range from 5 to 25 ng/mL. A common method for rapidly increasing 25-hydroxyvitamin D levels is an oral bolus (or “loading”) dose of vitamin D3. According to the European Society for Clinical Nutrition and Metabolism (ESPEN) Guideline on clinical nutrition in the intensive care unit, a single high dose of 500,000 IU (12.5 mg) of vitamin D3 appears safe for patients with deficiency during the first week of treatment. However, in critically ill patients, potential limitations on absorption and on liver function, and the four or so days it takes to hydroxylate the vitamin D3 into 25-hydroxyvitamin D, unacceptably delay the urgently needed improvement in immune function.
A more effective approach, as recommended by Prof. Wimalawansa, involves a single oral dose of calcifediol (25-hydroxyvitamin D) of 0.014 mg per kilogram body weight. For an average weight adult, this is approximately 1 milligram. Calcifediol is more readily absorbed than vitamin D3 and directly enters circulation, safely elevating levels above 50 ng/mL within just 4 hours. This boosted level decreases over days to a week, so further calcifediol or regular or bolus vitamin D3 supplementation is necessary to maintain it. A 1 mg dose of calcifediol is roughly equivalent to a modest 160,000 IU (4 mg) of vitamin D3. Unless there is reason to suspect the patient has excessive 25-hydroxyvitamin D, blood tests are unnecessary, as this intake does not lead to toxicity.
The proper solution to numerous acute and chronic health problems is to encourage and support – but not force – everyone to supplement vitamin D3 in sufficient quantities to attain at least 50 ng/mL 25-hydroxyvitamin D. For those who have not done this, and who are diagnosed with COVID-19, sepsis, or any other potentially deadly illness, the above calcifediol protocol is by far the most important medical intervention they urgently need, other than breathing and blood pressure support. Calcifediol is available in some European countries as inexpensive 0.266 mg prescription Hidroferol or Neodidro capsules. Bottles of 60 small d.velop 0.01mg tablets are available in the USA without prescription for $20.
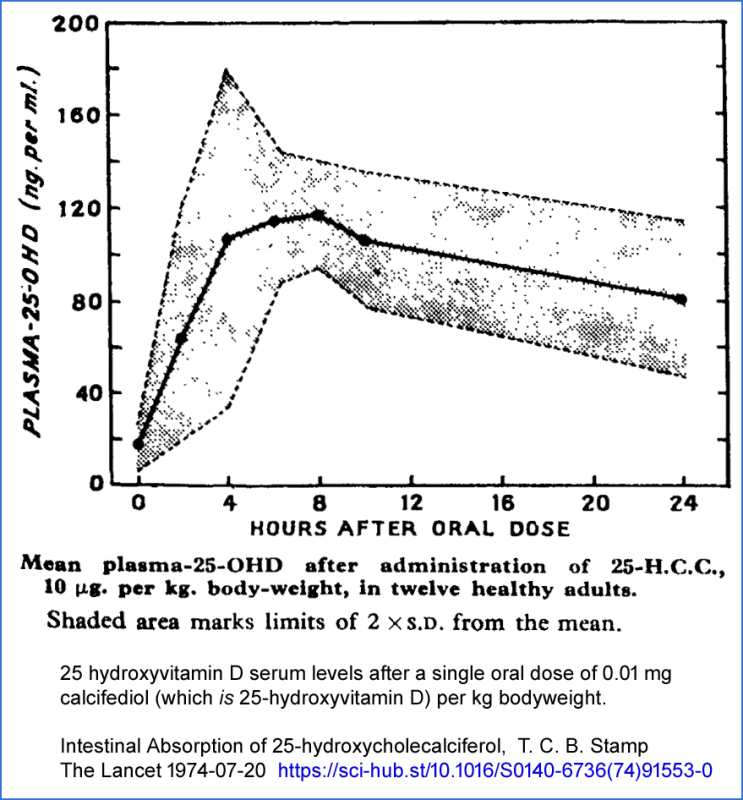
The graphs below contrast the typical, months-long rise in 25-hydroxyvitamin D with the 4-hour increase following a 0.532 mg dose of calcifediol in healthy subjects:
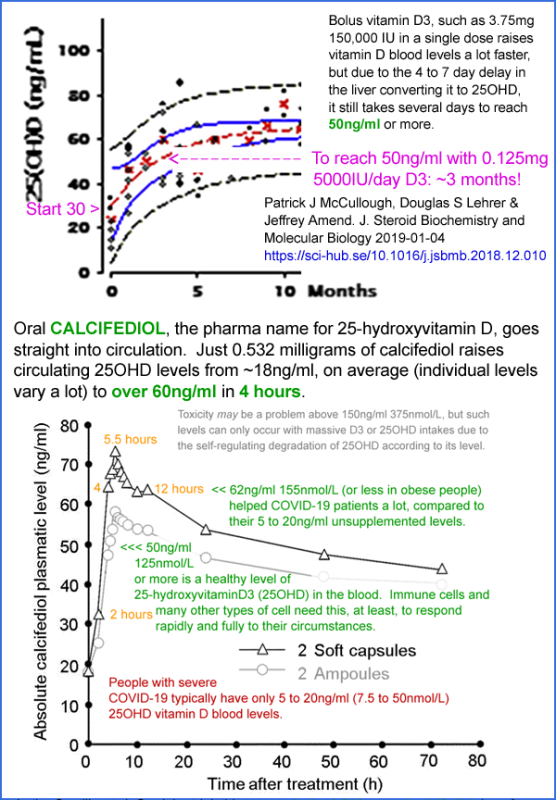
These graphs are from McCullough et al. 2019 and a 2016 patent for the capsules used in randomized controlled trial, reported in Castillo et al. 2020, which we discuss below. The Castillo et al. researchers knew that oral calcifediol would raise 25-hydroxyvitamin D levels more quickly than bolus vitamin D3 but might not have been aware of the patent or the 4-hour rise time. They later discovered a rarely-cited 1974 article by T.C.B Stamp (later, Sir Trevor) titled “Intestinal Absorption of 25-hydroxycholecalciferol” which depicts the rapid increase in response to a single 0.01 mg/kg body weight oral dose of calcifediol.
Many doctors’ understanding of vitamin D treatment for acute diseases is limited by:
- Not knowing that 50 ng/mL 25-hydroxyvitamin D is required for proper immune system function.
- Being unaware that even bolus doses of oral vitamin D3 take days to raise 25-hydroxyvitamin D levels.
- Lack of knowledge about how oral calcifediol attains this in 4 hours.
- A more fundamental misunderstanding that oral vitamin D3 will boost 1.25-hydroxyvitamin D levels, which is not the case, with these levels somehow “boosting the immune system”.
Research and a broader understanding of the importance of maintaining 50 ng/mL circulating 25-hydroxyvitamin D levels have progressed more slowly than they would have if all participants – particularly immunologists and doctors – had devoted the necessary attention to this field.
People with backgrounds in engineering, who are accustomed to the rapid pace of progress in areas like semiconductors and microprocessors, may find the slow advancement in this field surprising. They may also notice the apparent lack of interest many doctors display towards research that contradicts the consensus view among their peers.
In a world where all doctors and most people recognise the necessity of proper vitamin D3 supplementation for immune system health, the spread of the SARS-CoV-2 virus would likely have been prevented. Additionally, influenza and sepsis cases would be rare, and overall health would see significant improvements.
Vitamin D3 and calcifediol as an early treatment for COVID-19, sepsis etc.
It is not widely known that this calcifediol protocol will generally lead to rapid improvements in most cases of COVID-19, sepsis, and other acute illnesses where weak innate and adaptive responses – and wildly dysregulated inflammatory responses – harm and kill many people.
Doctors and immunologists should be interested in providing the immune system and the rest of the body with the conditions they need to function properly. However, for various troubling reasons, most are not. Two leading immunology textbooks, Janeway’s 9th Edition and Abbas’ 10th Edition, totaling 1500 pages, do not mention vitamin D in their indexes.
Vitamin D – as bolus vitamin D3 or better still, 0.014 mg/kg body weight calcifediol – should be recognized as the most effective early treatment for COVID-19. However, at the constantly updated meta-analysis site c19early.org, Vitamin D is rated as less effective, among the extensively studied early treatments, than ivermectin, a no-longer useful monoclonal antibody, quercetin, povidone-iodine, melatonin, fluvoxamine, and exercise.
This leads many clinicians to regard vitamin D as just another treatment in their extensive toolkit. Lacking the understanding mentioned above, they administer one or more drugs without the decisive calcifediol treatment that would enable most of their patients’ immune systems to function properly within hours – probably for the first time in their lives.
Vitamin D COVID-19 treatment randomized controlled trials (RCTs) are highly varied in terms of disease severity at intake, criteria for success, and treatment protocols. Many used ineffectual quantities of vitamin D3 in the first five days. All those that used 7.5 mg (300,000 IU) or more vitamin D3 produced good results, as did some of those that used less – but these were generally smaller trials and so accorded relatively little significance.
The most significant of these RCTs is Castillo et al. , published in August 2020. If those in charge of the pandemic response had taken full account of this research and had been solely devoted to suppressing COVID-19 transmission and severity – rather than focusing on the supposed essentiality of vaccines – they would have mounted a global campaign of vitamin D3 manufacture and distribution, with calcifediol for early treatment, by the end of that year. This approach, especially with early treatments involving zinc and inexpensive drugs, would have ended the pandemic without lockdowns, vaccines, or masks and with only a fraction of the current terrible death toll.
The researchers worked with 76 COVID-19 patients hospitalized in Cordoba, Spain, all of whom were treated with hydroxychloroquine and the antibiotic azithromycin. The 50 patients in the treatment group received a single oral dose of 0.532 mg calcifediol upon admission, followed by 0.266 mg doses on days 3, 7, 14, 21, etc.
The positive results were partly due to imperfect randomization, which resulted in the control group containing a significantly greater number of patients with co-morbidities. However, two MIT computational biologists analyzed the results in a preprint and concluded that the decreased ICU admissions were associated with the calcifediol intervention, warranting immediate, well-designed clinical trials to further evaluate the effectiveness of this treatment.
The results, even with these caveats, were dramatic: ICU admissions dropped from 50% to 2%, and deaths from 8% to zero. The initial 0.532 mg dose of calcifediol was about half that recommended in the above-mentioned 0.014 mg / kg BW protocol, which would have been 1 mg for a 70 kg patient.
In late 2020, with the world in a panic about COVID-19, with lockdowns being enforced and poorly tested mRNA and adenovirus vector quasi-vaccines about to be introduced, this important research should have been discussed and celebrated. However, to this day, few have heard of it. (Later research by the same team with calcifediol produced less dramatic results, but by then calcifediol was being widely used in the general population, the treatment protocol was more complex, compliance could not be ensured and these later trials had no proper control group.)
In conclusion, the calcifediol protocol’s potential in treating COVID-19, sepsis, and other acute illnesses is undervalued due to limited knowledge and understanding among medical professionals. Greater awareness and acknowledgment of vitamin D’s role in treatment, along with calcifediol’s rapid impact on patients’ immune systems, will change the landscape of healthcare in the face of pandemics and other critical illnesses. It is crucial to raise awareness of the importance of vitamin D3 and the calcifediol protocol in both medical education and clinical practice.
Sepsis, inflammation and lack of helminths
This deadly lack of understanding about the three vitamin D compounds and their role in the immune system, which prevented health authorities from halting the COVID-19 pandemic, resembles similar patterns of poor understanding of other diseases. Corruption by multinational pharmaceutical companies plays a significant role in suppressing knowledge of the importance of the vitamin D compounds beyond their function in calcium-phosphate-bone metabolism. Leading vitamin D researcher Bill Grant reported on this in his 2018 article: “Vitamin D acceptance delayed by Big Pharma following the Disinformation Playbook.” However, this cannot be the full explanation, as the same pattern exists in China, which is beyond the direct reach of Western multinationals.
Sepsis is an horrific condition in which an uncontrolled viral, bacterial, or fungal infection triggers an extreme, self-destructive inflammatory response, damaging organs and often proving fatal. Quick diagnosis is crucial but challenging, as patients may present a wide range of nonspecific symptoms and their condition can deteriorate rapidly.
Google Scholar finds 54,000 articles on sepsis and vitamin D, many indicating that sepsis patients tend to have even lower 25-hydroxyvitamin D levels than the general population. While infection and inflammation can lower this level, low pre-infection levels contribute significantly to the risk. However, the only vitamin mentioned on the Wikipedia page for sepsis is vitamin C.
Given this knowledge, it is clear that a 50 ng/mL 25-hydroxyvitamin D level would greatly reduce the risk of the pervasive infections that trigger sepsis, as well as reduce the likelihood of an excessive inflammatory response.
In immunology, the term “inflammation” has a broad meaning. It includes the recruitment of immune cells to infection sites and certain cytotoxic (indiscriminate cell-destroying) responses, such as those of eosinophils – the suicide bombers of the immune system. These cytotoxic responses evolved primarily to tackle multicellular parasites, like helminths (intestinal worms), since antibodies and macrophages that work effectively against cancer cells, bacteria, fungi, and viruses make little impression on pathogens composed of billions of cells.
A lesser-known, but well-established and only partly researched, cause of excessive, cell-destroying inflammation is the absence of helminths in humans – and in our companion and agricultural animals – in the last century or so. Helminths long ago evolved compounds that downregulate their hosts’ inflammatory responses. Our ancestors seem to have been ubiquitously infested with one or more species of helminth, and we have inherited their evolutionary adaptation to this: an overly-strong inflammatory response that would probably be balanced when downregulated by helminthic compounds.
Now that we are all de-wormed, we are prone to excessive inflammation. Some of us, due to genetic variation, have particularly strong responses which cause numerous autoimmune inflammatory disorders such as multiple sclerosis, rheumatoid arthritis, psoriasis, asthma, cluster headaches, and migraine. Please see vitamindstopscovid.info/06-adv/ and helminthictherapywiki.org for links to and discussion of helminthic therapy – in which these diseases can be suppressed by deliberate helminth infection. The first page also discusses the high 25-hydroxyvitamin D protocols of Cicero Coimbra and others, which can also suppress these conditions, with medical monitoring to guard against excessive calcium levels and bone loss.
The success of both these treatment regimes indicate that the lack of helminths is the fundamental problem underlying acute and chronic inflammatory disorders, with low 25-hydroxyvitamin D levels greatly exacerbating the excessively strong inflammatory response. The fields of vitamin D and helminth research are like ships passing in the night – unaware of each other. Coimbra protocol clinicians explain their success speculatively, using the term “vitamin D resistance”, without referring to helminths. Helminthic researchers do not mention vitamin D.
Helminthic modulatory compounds, such as tuftsin-phosphorylcholine, have been discovered and synthesized and are currently being researched. However, none are yet available for therapeutic use. It is easy to imagine these compounds being used judiciously, along with proper vitamin D3, boron, magnesium, zinc, and omega-3 fatty acid intakes, and avoidance of excessive omega-6 fatty acids, to successfully suppress many inflammatory disorders, including those that contribute to obesity, depression and neurodegeneration.
Kawasaki disease, MIS-C, PIMS and COVID-19
Kawasaki disease is an acute and potentially fatal inflammatory vasculitis that affects infants and primarily younger children. An infectious trigger is usually observed weeks or months before onset. Severe cases involve coronary artery aneurysms, which can turn deadly later in life.
Decades of Kawasaki disease research articles and clinical reports portray the etiology of the disease as a mystery. Upon learning well-known epidemiological characteristics of the disease, such as peak incidence in Japan in winter or predominantly affecting dark-skinned children in Paris, many non-specialists would suspect inadequate vitamin D as a significant causative factor. However, such ideas seem not to occur to most pediatricians.
In 2015, Italian researchers Stagi et al. published an article which should have transformed the understanding, prevention, and treatment of Kawasaki disease. Yet, by May 2020, it had been cited only13 times. Thankfully, there have been 39 citations in the following three years, but this is a small fraction of the impact it should have had.
The study involved 21 girls and 58 boys, with an average age of 5.8 years. Their average 25-hydroxyvitamin D levels were 9.2 ng/mL, while age-matched controls averaged 23.3 ng/mL. The average level of children who developed coronary artery abnormalities was even lower: just 4.9 ng/mL. At most, only a fraction of this difference could be explained by the disease depleting 25-hydroxyvitamin D levels. The rest of this strong discrepancy is clearly causative, along with genetic predisposition and the triggering infections.
Since these dangerously low 25-hydroxyvitamin D levels are easy to boost and should be raised for numerous other reasons, one might think that this research would have been a eureka moment for Kawasaki disease researchers and clinicians, portrayed in the mainstream media as a game-changing breakthrough. However, it has been largely ignored.
Kawasaki disease can now also be triggered by COVID-19 infections, including those that are asymptomatic, as is often the case with children. Two diagnoses related to Kawasaki disease emerged in 2020: MIS-C (Multisystem Inflammatory Syndrome in Children) and PIMS (Pediatric Inflammatory Multisystem Syndrome). These are triggered by COVID-19 infection or, occasionally, COVID-19 quasi-vaccination.
Kawasaki disease resulting from COVID-19 is part of a symptomatic continuum with MIS-C/PIMS, as described by Tsoukas and Yeung in 2022. Infants and younger children are more likely to be diagnosed with Kawasaki disease, while teenagers and young adults are more likely to be diagnosed with the other two conditions, which involve less vasculitis and more damage to organs.
One of us (RW) wrote to dozens of authors of Kawasaki disease/MIS-C articles in 2020 to raise their awareness of Stagi et al.’s research and the obvious implications for vitamin D3 as a preventive measure and calcifediol as treatment. Only one replied, stating without specific arguments that they could not imagine the problem being low vitamin D. A 2022 survey of 50 consecutive Kawasaki disease/MIS-C articles in Google Scholar found that only one mentioned vitamin D and then only in passing. The situation may have improved somewhat since then. Another set of emails to some of these pediatricians resulted in a single reply, this time much more appreciative, from a doctor who had not previously considered vitamin D.
In conclusion, the lack of understanding and the underutilization of vitamin D in the prevention and treatment of various inflammatory disorders, such as sepsis and Kawasaki disease, have led to the acceptance of very high levels of suffering, harm and death as normal and inevitable, when the great majority of it could be prevented with proper nutrition. Sepsis alone is like a monster chewing through humanity at the rate of World War II or COVID-19, all day, every day – one death every 3 seconds.
The integration of vitamin D research with helminth research could open up new avenues for more effective treatments, potentially saving lives and improving the quality of life for those affected by these conditions.
Beyond corruption, or ordinary levels of incompetence
Corruption accounts for only a portion of the severe lack of awareness within the medical profession regarding the importance of maintaining adequate 25-hydroxyvitamin D levels for proper immune system function. The evidence provided in the research and reviews cited above suggests that low 25-hydroxyvitamin D levels are a significant factor contributing to the transmission and/or severity of COVID-19, influenza, sepsis, KD, MIS-C, PIMS, and numerous autoimmune inflammatory disorders. Nevertheless, the public remains reliant on the majority of doctors and immunologists who are largely unaware of this.
These medical professionals are not dim-witted, incompetent, or of poor character. Like everyone else, their ability to recognize the systemic shortcomings within their own and their profession’s understanding of the world is constrained by groupthink. Some doctors manage to free themselves from this mindset, only to face immense difficulty in getting their colleagues to consider this vital information. Such doctors can be ostracized and derogatorily referred to by their peers. Similarly, those who criticize quasi-vaccines and the suppression of ivermectin and other genuinely safe, effective, and inexpensive treatments for COVID-19 face retribution, including deregistration.
These detrimental patterns in medicine, which discourage innovation and trap most practitioners in a cycle of corrupted groupthink and ineptitude, seem to target low-key, unglamorous solutions to pressing medical problems currently addressed by expensive, sophisticated interventions. Profit motives are obviously at play here. Another possible factor is that most doctors did not endure a decade or more of demanding, costly training simply to spend their careers repeatedly advising patients to take vitamins, avoid excessive omega-6 fatty acids, sugar, and salt, and to exercise more. Part of this resistance may stem from many patients expecting more narrowly targeted and sophisticated treatments, considering the cost of medical services.
Industries that celebrate innovation – such as biotechnology, electronics, and software – rarely experience the majority of their professionals being mired in unproductive stagnation for years, as occurs in medicine. There is innovation in medicine, evidenced by routine eye, hip, and knee surgeries that would have seemed miraculous a few decades ago. Dental care has also seen extraordinary advancements.
Entire fields of medicine fall victim to misguided admiration for complex, sophisticated, and crowd-driven deviations from what patients and the public genuinely need. Simpler approaches, which are precisely what they require, are often disregarded, shunned, or ridiculed as unworthy of doctors’ attention.
Unrealistic, sometimes quasi-religious, hopes and expectations surrounding vaccines have arguably been the most significant distortion of thought and practice during the COVID-19 pandemic. If no such vaccines had been possible or if they had been quickly and correctly dismissed as having limited or negative value, doctors and other professionals would have been forced to rely on early treatments and nutrition. These would have been far more effective than the treatments widely referred to as COVID-19 vaccines, but would not have satisfied certain professionals’ desire to incite panic and to control entire populations during a manufactured crisis.
The vitamin D complex of medical no-go zones would likely collapse if even one aspect were rectified. For example, if all pediatricians recognized the importance of proper vitamin D3 supplementation, in-utero and beyond, for reducing the incidence of Kawasaki disease, MIS-C, PIMS, pre-eclampsia, autism, schizophrenia, and pre-term birth, then the other no-go zones would crumble – sepsis, COVID-19, influenza, and eventually neurodegeneration. Few doctors are interested in, or aware of, the fact that people with Parkinson’s disease exhibit even lower 25-hydroxyvitamin D levels than those without the disease, even before displaying symptoms.
Further examples of persistent medical avoidance of information that would lead to simpler, more effective, less glamorous, and less profitable solutions to major health problems include:
- Peer reviewed research in 2011 by M. R Naghii et al. demonstrates that a daily 10 mg supplemental boron intake causes ultrasound-confirmed kidney stones to disintegrate, allowing them to be passed more easily, often within days of beginning treatment. Naghii recommends that L-arginine significantly aids this process. Consequently, most of the multi-billion-dollar kidney stone treatment industry may be both unnecessary and harmful, given its financial costs and medical risks compared to consuming half the safe limit of boron per day.
- Boron should be recognized as an essential nutrient with healthy daily intakes around 10 mg, instead of the typical ~1 mg, mainly from fruit and vegetables grown in boron-depleted soil. Benefits include alleviating rheumatoid arthritis and enhancing dental and bone health (Nothing Boring About Boron, 2015 PMC4712861 and aminotheory.com/cv19/#08-boron).
- Restless Legs Syndrome / Periodic Limb Movement Disorder and their sub-diagnosable variations causing insomnia can be readily explained by several common dietary and lifestyle choices, many of which can be avoided without medical intervention. These reduce inhibitory dopaminergic and/or opioidic receptor activation in spinal reflex circuits responsible for a uniquely human, soft-touch-activated, foot arch protective, reflex response. Despite notifying RLS.org and major RLS researchers of this in 2011, there has been no response, and the etiology remains officially unknown. Millions of sufferers continue to be treated with personality-altering dopamine antagonists and, when these fail, opioids.
The scourge of COVID-19, sepsis, and other related issues will only be eradicated once the majority of doctors understand the immune system’s need for 50 ng/mL 25-hydroxyvitamin D. This will largely depend on immunologists, who currently appear so engrossed in the intricacies of cytokines, genetic variations, and antibody types that they cannot fathom that nearly their entire profession has not understood a critical mechanism by which individual immune cells respond to their changing circumstances.
Seasonality of influenza and COVID-19
Healthy 25-hydroxyvitamin D levels of 50 ng/mL or higher only slightly decrease the likelihood of COVID-19 infection from any given viral exposure. These levels offer strong protection against severe disease. Even more crucial for entire populations, such levels enable full-strength immune responses that rapidly suppress viral infections and reduce average levels of viral shedding. This mechanism, more than any other, decreases transmission and, consequently, the total number of infected individuals. The robust immune response also results in optimal, long-lasting immunity against the same or similar pathogens.
Modest but significant changes in population average 25-hydroxyvitamin D levels serve as the primary driver of influenza and COVID-19 seasonality: nutritionmatters.substack.com/p/covid-19-seasonality-is-primarily. As demonstrated in this article, the number of hospitalized COVID-19 patients in the UK declined exponentially from 19,617 in mid-April 2020 to 795 in late August. This monthly halving was primarily due to the summer peak in average 25-hydroxyvitamin D levels for individuals who do not adequately supplement with vitamin D3: around 25 ng/mL for whites and approximately15 ng/mL for those with dark or black skin. There were no lockdowns, vaccines, or widespread masking and social distancing measures during this time. Infection and hospitalization rates increased in September and the following months as 25-hydroxyvitamin D levels dropped and a new, more transmissible variant emerged.
Dror et al. and other reports
The graph at the start of this article displays histograms of population distribution of 25-hydroxyvitamin D levels. Firstly, in gray, are levels calculated from Luxwolda et al. 2012, which is the only study to date that has measured 25-hydroxyvitamin D levels in traditionally living Africans – 35 Maasai pastoralists and 25 Hadzabe hunter-gatherers in Tanzania, with an average age of 35. The mean level was 46 ng/mL (125 nmol/L). It is reasonable to assume that the immune systems of all humans today differ little from those of our African ancestors 50,000 years ago. However, adaptations have evolved since then, especially the loss of UV-B absorbing melanin among those who ventured far from the equator, which has enhanced many populations’ ability to generate vitamin D3 when exposed to UV-B light.
The other four histograms are from a September 2020 preprint by Israel et al., “The link between vitamin D deficiency and Covid-19 in a large population.” These are based on measurements made between 2010 and 2019 and recorded in an Israeli 4.6 million patient database. The mean levels are all much lower than 50 ng/mL. Despite living in sunny Israel, at 32° north – level with San Diego and Savannah, Georgia – the levels of Arab women are alarmingly low. Without proper vitamin D supplementation and considering their sun-avoidant lifestyle, the prospects for these women’s health – and their children’s neurodevelopment – must be bleak. Their median level is around 10 ng/mL.
Multiple UK research articles show that the median levels for Asian (Pakistani, Indian, and Bangladeshi) men and women in the UK are 10 ng/mL or less – and it is reasonable to assume that the median for the women would be significantly lower than this.
Israel et al. found greater rates of SARS-CoV-2 infection among those with low 25-hydroxyvitamin D levels, especially among women, whose levels are marginally or decisively lower than those of men of the same ethnic group. In addition to lower levels likely increasing the chance of infection, the most significant mechanism underlying this correlation may be that most individuals in the three ethnic groups, with progressively lower mean 25-hydroxyvitamin D levels – General, Ultra-Orthodox, and Arab – spend most of their time among other members of their group. These lower levels will lead to progressively weaker immune responses and, therefore, greater levels of viral shedding and transmission within those ethnicities. Family size and work practices – such as the ability to work from home vs. high public contact jobs – likely also play a role in these differing infection rates.
We now return to Dror et al.’s findings and those of other researchers who report such consistent and strong associations between low 25-hydroxvitamin D and COVID-19 severity that the former must be very largely causative of the latter, with obvious implications for how individual infections and the entire pandemic should be handled.
The records of 1,176 patients aged 18 and over, with two independent PCR-positive tests, who were admitted to a large hospital in northern Israel between 2020-04-07 and 2021-02-04, were examined for 25-hydroxyvitamin D blood test results measured 14 to 730 days before diagnosis. The maximal disease severity during hospitalization of the 253 patients with such test results were included in this prospective research study, stratified into mild, moderate, severe, and critical categories.
The researchers developed an algorithm for adjusting these levels to compensate for seasonal variation. However, the levels in the above graphs represent uncorrected, most recent, actual measured levels.
Mean ages across mild to critical severity categories were 53, 64, 72, and 76. In these categories, the mean BMIs were 27.5, 27.6, 29.2, and 32.0, respectively; death rates were 0%, 1.2%, 35%, and 85%; and mean 25-hydroxyvitamin D levels were 36, 19, 13, and 12 ng/mL. While 25-hydroxyvitamin D levels were inversely correlated with age, and age was correlated with severity, when subjects were stratified into three age ranges, 25-hydroxyvitamin D levels remained strongly and significantly (p < 0.001) inversely correlated with disease severity (Fig. 3).
A total of 61% of patients were Arabs. Among these, 64.3% had 25-hydroxyvitamin D levels below 20 ng/mL, compared to 36% for non-Arabs. Factors potentially contributing to vitamin D deficiency among Arabs include darker skin pigmentation, which decreases dermal vitamin D synthesis, and a preference for conservative dress in some cultures and religious societies, particularly among women, which further reduces skin exposure to sunlight and so lowers serum vitamin D levels. Despite the p = 0.006 significance of the disparity between Arabs and non-Arabs in 25-hydroxyvitamin D levels, the correlation of Arab ethnicity with respect to disease severity was low and not statistically significant: p = 0.3.
No data was available on vitamin D3 supplementation. However, it is reasonable to assume that most individuals with levels above 40 ng/mL were supplementing and/or had recent, extensive UV-B skin exposure at the time their blood was drawn. In the supplementary dataset, the three highest outlier 25-hydroxyvitamin D levels in the Severe category ranged from 56 to 67 ng/mL. These three patients were all 65 years or older and had both COPD and hypertension. Two of them died. These healthy levels, more than twice the population and patient average, reduce risk but cannot guarantee health or survival in all circumstances. Of the 38 patients who died, one was under 50 and a second was between 50 and 64, with 25-hydroxyvitamin D levels of 16 and 26 ng/mL, respectively. Among the other 36 who died, all aged 65 and over, the outlier 25-hydroxyvitamin D levels were 67, 56, and 35 ng/mL, with all three patients suffering from COPD and hypertension. Of the remaining 33 patients who died, the outlier 25-hydroxyvitamin D levels were 21 and 18 ng/mL, with the remaining 32 patients having had levels between 6 and 14 ng/mL, with a mean of 9.9 ng/mL.
The risks of hospitalization and serious harm resulting from low 25-hydroxyvitamin D levels are much more acute than depicted in the above graph, as those who are hospitalized generally have lower levels than those who are not.
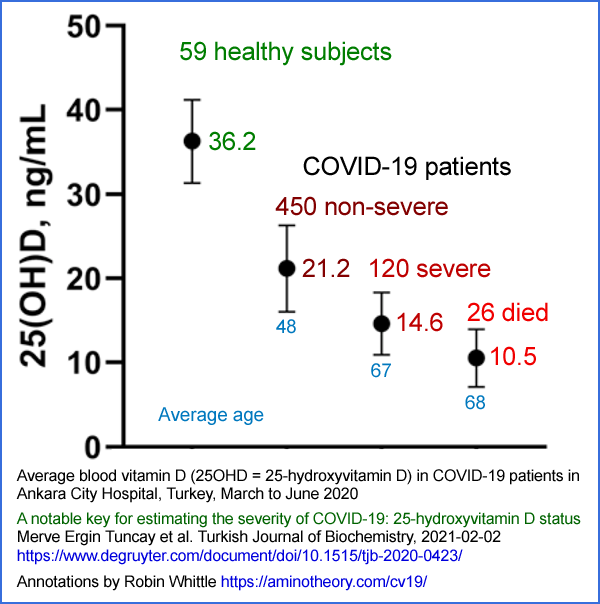
A February 2020 article by Tuncay et al. investigated the 25-hydroxyvitamin D levels of 596 PCR-positive COVID-19 infected patients and 59 healthy individuals in Ankara City Hospital, Turkey, from March to June 2020. This annotated version of their Fig 1 illustrates the strong, statistically significant (p < 0.001) relationship between low 25-hydroxyvitamin D levels and disease severity.
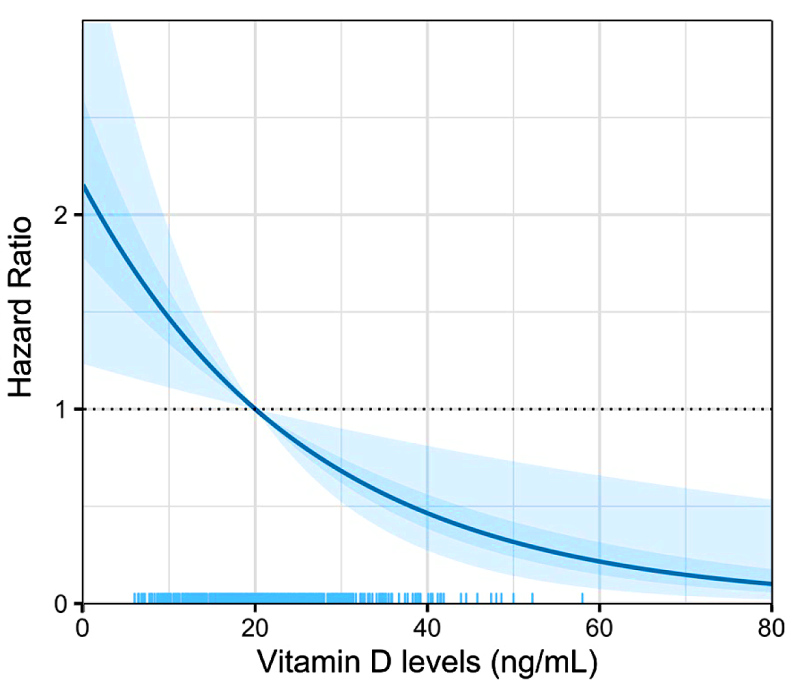
In a March 2021 preprint analyzing 551 patients in Mexico City from March to May 2020, Vanegas-Cedillo et al. reported that the increased risk of COVID-19 mortality conferred by low vitamin D levels was independent of BMI and epicardial fat. After adjusting for age, sex, BMI, C-reactive protein, epicardial fat, D-dimer, oxygen saturation, type 2 diabetes, and chronic kidney disease, they produced this modeled graph of risk of death as a function of 25-hydroxyvitamin D level, with 1 standardized to the risk at 20 ng/mL, which was close to the median for their sample.
Also in March 2021, Bayramoğlu et al. reported the mean 25-hydroxyvitamin D levels of 103 children, with an average age of 12, who were diagnosed with COVID-19 in an Istanbul hospital between March and May 2020. Those under 1 year of age and those with comorbidities (diabetes, asthma, tuberculosis, chronic renal failure, etc.) were excluded from the study. The divergence of mean levels was statistically highly significant (p < 0.001):
- 16 ng/mL for asymptomatic children.
- 14 ng/mL for children with mild symptoms.
- 10 ng/mL for children with moderate to severe symptoms.
They also reported similarly significant correlations between low 25-hydroxyvitamin D levels and low lymphocyte count, as well as high levels of inflammatory markers: C-reactive protein and fibrinogen. In adult cardiac patients, the levels of these two compounds are positively correlated with heart attack and death.
In a May 2021 BMJ article, Derren et al. identified 18 children aged between 4 months and 15 years, diagnosed with PIMS-TS (pediatric inflammatory multisystem syndrome temporally associated with severe acute respiratory syndrome coronavirus 2) between April 12 and June 25, 2020, in a children’s hospital in Birmingham, UK. Centrally located in the British Isles, its latitude of 52.5° north would place this city 240 miles north of the United States border if it were located in Western Canada.
These children were previously healthy, with no comorbidities. None of them died, but four required invasive mechanical ventilation, and one needed hemofiltration for renal failure. Sixteen of the children were Black, Asian, Minority Ethnic (BAME), and the other two were of White British Ethnicity. The mean 25-hydroxyvitamin D level on admission for the BAME children was 7.6 ng/mL, and for the White children, 24 ng/mL. A 2016 UK survey of children aged 4 to 10 found a mean 25-hydroxyvitamin D level of 21.6 ng/mL. The significance of the difference between this and the whole group’s mean level of 9.6 ng/mL was p < 0.001. The 12 children who were admitted to pediatric intensive care had lower mean 25-hydroxyvitamin D levels than those who were not. All of these 12 had abnormal (< 55%) left ventricular ejection fraction.
Echocardiagram examination of their coronary arteries showed that five had “prominent”, meaning dilated, arteries and one had fusiform dilation, in which the arterial walls are weakened and the vessel balloons to more than 150% of its normal diameter. The two children who had what the researchers considered to be “sufficient” 25-hydroxyvitamin D levels (20 ng/mL or more) had no such heart damage.
Footnote: In April and May 2020, three preprints purporting to be genuine research articles regarding vitamin D and COVID-19 were widely read and cited. Their first authors’ names were Alipio, Raharusun(a), and Glicio. The first name is of one of the fraudsters, who launched these as part of a completely fabricated series of 23 or so preprints. The other two names are fictitious. The details of this campaign are at researchveracity.info/alra/. Two of the fraudsters’ dupes, who raised funds for them, were given fictitious data which they transformed into a graph showing an improbably steep relationship between 25-hydroxyvitamin D levels and mortality. No proper effort was made to remove citations of this fake graph, and a copy of it remains to this day and is discussed in a video at www.powerofd.org.
Solutions to nested, strongly socially and institutionally embedded, problems
Researchers and clinicians who recognize the significance of optimal 25-hydroxyvitamin D levels for numerous aspects of health, beyond calcium-phosphate-bone metabolism, have dedicated years or even decades to raising awareness among their colleagues. Multiple interlocking barriers seem to hinder the natural and professional interest these colleagues should have in something so fundamentally crucial to human health. These barriers include:
- Utilization of the International Unit for vitamin D3 supplemental quantities (using the term “dose” implies medical treatment, whereas we are primarily discussing routine nutrition). Standardized to 1/40,000,000 of a gram in the early 20th century, this measure approximates the daily amount of vitamin D a baby rat needs to avoid developing rickets. This results in large numbers for healthy supplemental quantities, which can cause both clinicians and the public to be overly cautious about appropriate supplementation.
- Frequent repetition of the misleading statement that “vitamin D is a hormone”, even by leading vitamin D researchers. This seems to be an attempt to give cholecalciferol a gravitas that they believe it lacks as a mere vitamin. The term “secosteroid hormone” may be employed for added emphasis.
- Official guidelines for vitamin D3 supplemental intake do not account for body weight and obesity, providing only about 15% of what average weight adults need to achieve what we now know are healthy 25-hydroxyvitamin D levels.
- Misconceptions such as “vitamin D rich foods” and claims made about fortified foods can give some individuals a false sense of security regarding their vitamin D status. Fortified foods alone cannot achieve anywhere near 50 ng/mL circulating 25-hydroxyvitamin D. One of us (RW) contends that every effort that could be made to increase D3 food fortification would be better directed towards supporting proper voluntary supplementation.
- In countries such as Australia, the maximum quantity of vitamin D3 in retail supplements is an impressive-sounding 1000 IUs, equivalent to 0.025 mg. This is only 20% of what average weight adults require daily. The cost and inconvenience of consuming five of these a day poses significant barriers to proper nutrition. In the USA, 1.25 mg 50,000 IU capsules are more widely available and offer a more convenient and affordable alternative.
- Vitamin D is typically found on supermarket shelves between vitamins C and E, both of which have been overhyped.
- The majority of vitamin D3 production takes place in China for agricultural animals such as pigs, cattle, and poultry raised intensively indoors. Only a few plants, located in India and Europe, manufacture and refine it to pharmaceutical grade. The highly competitive USD$2.5k per kg price reflects the complex process of creating 7-dehydrocholesterol from wool fat, breaking one of its carbon rings with UV-B light from multi-kilowatt, specially doped, liquid-cooled mercury vapor lamps, and refining the product from benzene solution. These factories – none owned by major pharmaceutical companies – have minimal profit margins to invest in promotion, particularly since the cost of their product for each adult is approximately one cent per month.
- Regulatory capture by the pharmaceutical industry favors the development, approval, and marketing of novel drugs, vaccines, and monoclonal antibodies over the nutritional support most people need to maintain good health.
- The vast, global medical and biological research industry often overlooks vitamin D, as funding is typically directed toward more exotic projects.
- No peer-reviewed journal article provides an introductory explanation of 25-hydroxyvitamin D intracrine and paracrine signaling. In its absence, many researchers and clinicians assume the hormonal model of calcium-phosphate-bone metabolism also applies to “vitamin D” – implicitly 1,25-dihydroxyvitamin D – somehow “regulating” the immune system. This leads to many newcomers to the field perpetuating the problem by writing further uninformative and potentially misleading articles.
- While strong support has existed among leading researchers since the late 2000s for approximately 50 ng/mL circulating 25-hydroxyvitamin D, no consensus recommendation has been published for vitamin D3 supplemental quantities, as ratios of bodyweight, with higher ratios for those suffering from obesity, which will reliably achieve this for people of all ages and body morphologies without medical supervision.
As long as most people’s 25-hydroxyvitamin D levels remain at their current alarmingly low levels, no amount of effort with vaccines, monoclonal antibodies, antiviral drugs, lockdowns, or masks will suppress SARS-CoV-2 or protect all those who are infected by this or similar pathogens from severe harm or death. Other nutrients and affordable drugs have roles to play, but none can compensate for the weakened, often crippled, and destructively inflammatory immune responses in the general population caused directly by insufficient 25-hydroxyvitamin D.
The solution to COVID-19, sepsis, and influenza is population-wide, government-supported but unforced, vitamin D3 supplementation to achieve healthy 25-hydroxyvitamin D levels. There is no other solution. All other efforts in the absence of this repletion would be merely fiddling at the margins.
While issues such as corruption, censorship, government overreach, quasi-vaccine ineffectiveness and injury, and other arguably criminal aspects of the pandemic response must be discussed and addressed, these have distracted from raising awareness and improving understanding of the immune system’s need for 50 ng/mL circulating 25-hydroxyvitamin D.
Inadequate 25-hydroxyvitamin D has been a problem for a growing fraction of humanity since modern humans moved far from the equator around 40,000 years ago. Biological and industrial approaches to synthesizing vitamin D3 all involve approximately 297 nm UV-B light, which also breaks bonds in DNA and raises the risk of skin cancer. Pigmentation to reduce this damage leads to reduced vitamin D3 production, particularly during periods of low UV-B flux.
Housing, vehicles, clothing, and now sunscreen have all attenuated cutaneous vitamin D3 production in most countries. Solving the COVID-19 problem depends on solving the 25-hydroxyvitamin D problem, which is part of a longstanding reluctance among the majority of those most responsible for this aspect of proper nutrition – doctors and immunologists – to take an interest in information that demonstrates they have been mistaken for decades about the necessity for proper vitamin D3 supplementation.
The primary barrier to solving this problem is groupthink – the natural tendency we all have to consider information that seems to contradict the consensus views of those we most trust as being unworthy of our attention.
The greatest challenge in repleting everyone’s 25-hydroxyvitamin D may be that the intervention involves an easily understood mechanism of action of a readily available nutritional supplement with which most people are already somewhat familiar. This is especially true during a time of crisis, with entire professions working diligently with billions of dollars in funding to developing solutions that are widely believed to be necessarily disease-specific, spear-like, and narrowly targeted.
Professor Wimalawansa, who has energetically researched and promoted awareness of vitamin D since the mid-1990s, told one of us (RW) that the most common response from doctors to his efforts is: “How could it be true? It’s too simple.”
Addressing the widespread deficiency in 25-hydroxyvitamin D levels is crucial to combating not only COVID-19 but also other illnesses related to immune system function. It is imperative that doctors, immunologists, and public health officials recognize the significance of proper vitamin D3 supplementation and work towards implementing effective strategies to ensure adequate 25-hydroxyvitamin D levels in the general population.
Only by overcoming current patterns of groupthink and embracing the simplicity of this solution, will it be possible to make significant strides in the battle against COVID-19 and other infectious diseases. With a concerted effort to raise awareness about the importance of maintaining healthy 25-hydroxyvitamin D levels, there is hope for a more effective approach to public health and disease prevention.
This article appears at the authors’ Substacks https://www.drgoddek.com and https://nutritionmatters.substack.com, both of which enable comments and further discussion.
Join the conversation:

Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.










