A directive to health practitioners barring criticism of the Covid vaccines and rollout has finally been dropped by Australia’s medical regulator, AHPRA.
On 9 March 2021, AHPRA and the National Boards published a joint statement to help health practitioners “understand what’s expected of them in giving, receiving, and advising on and sharing information about COVID-19 vaccination.” This has now been superseded by a general information page on vaccination.


The statement was controversial because it appeared to expressly prohibit health practitioners from disclosing to patients the risks and the poor quality (or total lack) of evidence for effectiveness and safety of the Covid vaccines. It also implied a ban on critising policies around the rollout, including workplace vaccination mandates.
Per the statement, “There is no place for anti-vaccination messages in professional health practice, and any promotion of anti-vaccination claims including on social media, and advertising may be subject to regulatory action.”
This was not an empty threat. In the first year of the Covid vaccine rollout (2021-22) AHPRA suspended 21 health practitioners and investigated many more in response to 1,300 notifications relating to Covid and the vaccines.
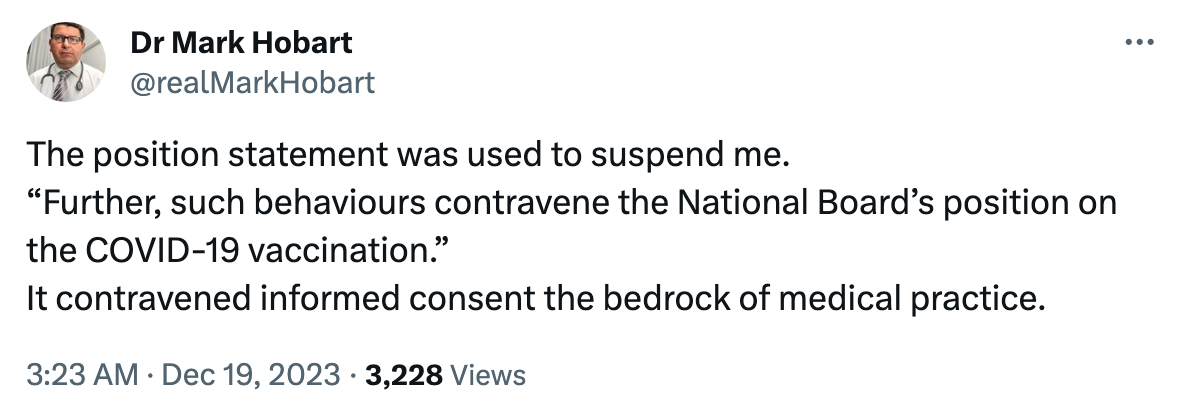
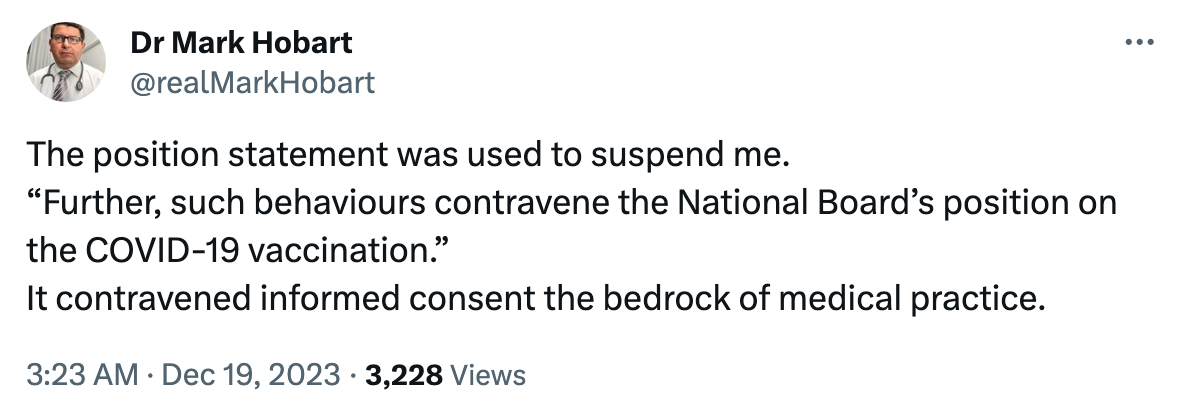
Investigations could be initiated for minor ‘offences,’ such as posting political content and general information about holistic health, as in the case of Dr Sally Price. Suspensions were issued for more serious contraventions of AHPRA’s position statement, such as issuing medical exemptions to patients, in the case of Dr Mark Hobart and Dr Duncan Syme, or prescribing ivermectin off-label, as did Dr My Le Trinh (all three doctors remain indefinitely suspended).
Dr Syme said of the suspension process, “The process is the punishment… While you’re [suspended] under investigation, you cannot earn a living. So, doctors are scared into toeing the line because you can’t risk getting investigated.” Though Dr Price was not suspended, she described the investigation process as “destructive” and “very stressful.”
In some cases, health practitioners have been driven to suicide during the process. Earlier this year, AHPRA released a confronting study revealing that between January 2019 to December 2021, 16 health practitioners had taken their own lives while subject to investigation by the regulator, with another four attempting suicide or self-harming.
Practitioners felt that AHPRA’s position statement, and its hawkish enforcement of it, had created a culture of fear and silence in the medical profession that put patients’ lives at risk.
When GP and former president of the Australian Medical Association (AMA) Dr Kerryn Phelps publicly announced her Covid vaccine injury in December 2022, she claimed that AHPRA had censored discussion about adverse events related to the vaccines, “with threats to doctors not to make any public statements about anything that ‘might undermine the government’s vaccine rollout’ or risk suspension or loss of their regulation.”


Dr Christopher Neil, President of the Australian Medical Professionals Society (AMPS), said that AHPRA had created “a Star Chamber effect,” and that the March 2021 position statement was at the root of a “dangerous shift in Australian medicine,” in which doctors were becoming increasingly beholden to governments and bureaucrats instead of the individual patient.
Dr Price arrived at the same conclusion after being required to undergo professional re-education as part of her investigation process, which involved studying the AMA Code of Ethics. She said that she was, “struck by how AHPRA’s position statement overrode our professional ethics,” making it “impossible” for doctors to provide valid informed consent to patients. Dr Syme characterised the bind as a Hobson’s choice: “Are you going to protect yourself or protect your patient?”
Dr Hobart stresses that the position statement was in breach not just of medical ethics, but of the law. “That position statement contravened the legally accepted basis for informed consent which is the High Court case of Rogers v Whitaker, in which the High Court stated the doctor must tell the truth to the patient. AHPRA was intruding into the doctor-patient relationship through undue influence, preventing the doctor from telling the full truth about the vaccine. That’s why doctors didn’t give exemptions – for fear of suspension.”
Now that AHPRA’s position statement on Covid vaccination has been superseded, there are no explicit directives to health practitioners within the vaccine information guidelines preventing them from discussing the downside of Covid vaccination, as well as the benefits, with their patients. But this may not mean that health practitioners are free to provide informed consent in practice.
When asked to clarify the differences between the superseded (2021) position statement and the new one, a spokesperson for AHPRA advised,
“During the pandemic Ahpra issued guidance to help practitioners understand how these obligations related to the public health orders that were in place at that time. The obligations on practitioners remain the same, however the public health orders have changed – so our statement has as well.”
“The 2021 position statement didn’t publish new information, nor did it include new requirements of practitioners. It drew together existing information from the codes and guidelines and took into account public health advice at the time. We collated this information to provide practitioners with clear guidance on their obligations at the time.”
Despite the superseded direction on Covid vaccination specifically, Dr Price does not believe anything much will change. “If anything, it seems to be bits and pieces of rewording, and more reliance on businesses and institutions to apply the pressure,” she says. “For example, hospitals and medical centres will not allow health professionals to work unjabbed, as is still occurring.”
Dr Hobart thinks that AHPRA “may be worried” because, “what they did was stop doctors from warning people about the vaccine, and some of those patients have died. That is the bottom line, that’s how bad it is. I think they’re starting to face up to this. They’re not going to be able to keep this under the table forever. People are going to be angry.”
Certainly, Dr Hobart is still angry. After more than two years on the bench with his suspension, he has been in and out of the courts trying to get AHPRA to reach a decision about his medical registration. On 20 December, Dr Hobart served AHPRA with papers to take them to the High Court in the hopes of initiating a judicial review. “When they suspend a doctor they can’t just do nothing for two years,” he says.
Unlike Dr Hobart, Dr Price is no longer interested in fighting within the system. After her investigation and re-education, Dr Price allowed her registration with AHPRA to lapse, saying she “want[s] no part” of the system that she believes has “become a wasteland.” Dr Price is now directing her energy towards exploring new opportunities working towards “health literacy and sovereignty,” which she believes are “important aspects of the future of well-being.”


For health practitioners who choose to remain in the system, and who are concerned about medical censorship in Australia, the softening of the AHPRA position statement is a small win, but there is still a long way to go.
A spokesperson from AMPS says of the updated position statement,
“There has not yet been a real reckoning for the way in which the 2021 position statement and regulatory actions of AHPRA impacted on the free speech of doctors, the doctor-patient relationship, and informed consent.
“We welcome the omission of overt threats from regulator in the new position statement, however there are still substantial concerns about the regulatory environment in Australia, which remains hostile to individualised care.”
Next year, the implementation of changes to the National Law threatens to further silence doctors on matters that could affect confidence in public health initiatives. Both AMPS and the AMA are opposed to the changes, which the AMA argues “will have major impacts on the lives and work of medical practitioners without improving standards of care for patients.”
AMPS has drawn up a Health Reform Declaration to which medical professionals can put their name, calling for “the restoration of informed consent” to the profession, and an ongoing Stop Medical Censorship campaign has attracted considerable public interest.
“It’s simple,” says Dr Hobart. “AHPRA and the Medical Boards need to adhere to the law and our code of medical ethics.”
Republished from the author’s Substack
Join the conversation:


Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.









