As the West drifts further and further away from optimal public health systems, let us dream out loud about what an ideal set of institutions to promote health would look like.
The covid debacle has revealed the depths of perversity that our health bureaucracies, both public and private, have plumbed. We’ve seen in graphic detail how most of the agencies created to protect our health have gone rogue, and we’ve seen up close the malign influence of Big Pharma, now deeply embedded in public health agencies and using its privileged position to sideline cheap, effective medicines in order to peddle expensive poisons. Sadly, all of this in many ways is just the tip of the iceberg.
Two of us have worked as health economists and institutional designers for over two decades, advising several governments about well-being and mental health systems. We have also written papers and books on corruption in health and other sectors. What we have seen leads us to radical conclusions about both the prognosis for the present systems, and the remedy for societies that truly wish to promote the health of their populations.
The Public Health Disaster in Two Statistics
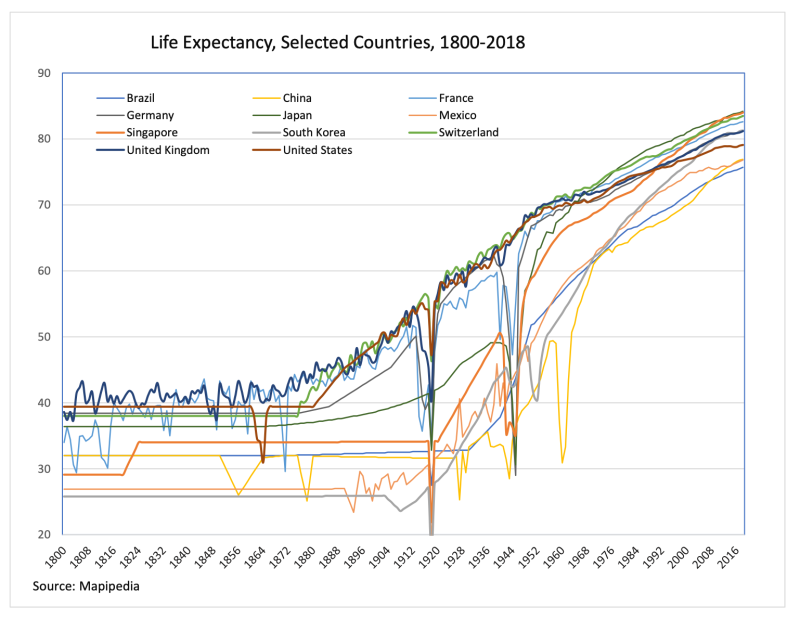
Two statistics together tell a sobering story about the depth of the health-related problems now faced in the West: life expectancy and spending on health over time. The logical expectation is that more of the latter should produce greater gains in the former.
Below we graph changes in life expectancy from 1970 to 2021. While Africa is in a league of its own, Asia and Latin America (and belatedly Eastern Europe, after its untethering from the Soviet bloc and marriage to the European Union) have been steadily closing the gap on the rich Western countries. Between 1970 and 2021, the US has added six years to its life expectancy and Western Europe 10, while Asia has added 19 (China added 22) and Latin America 14. Africa added 17 years but from a very low base: its life expectancy in 1970 was only 45 years.
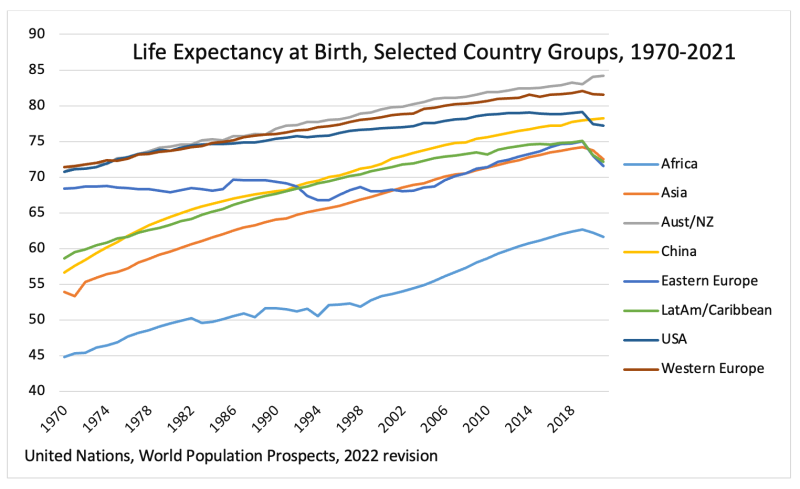
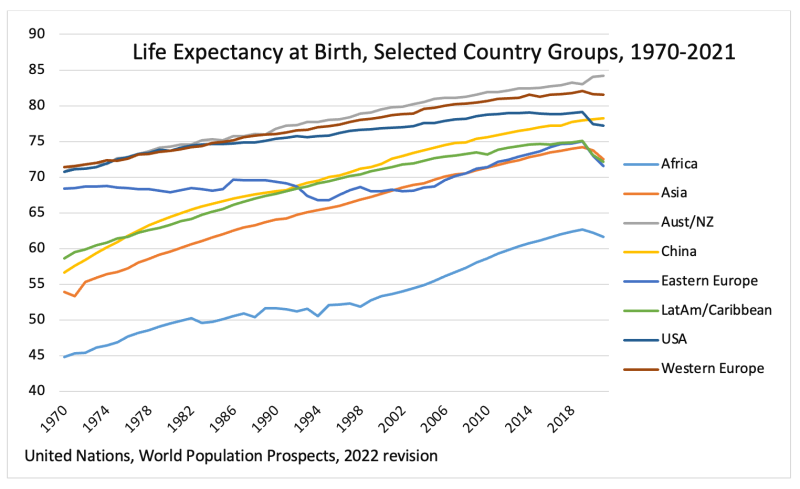
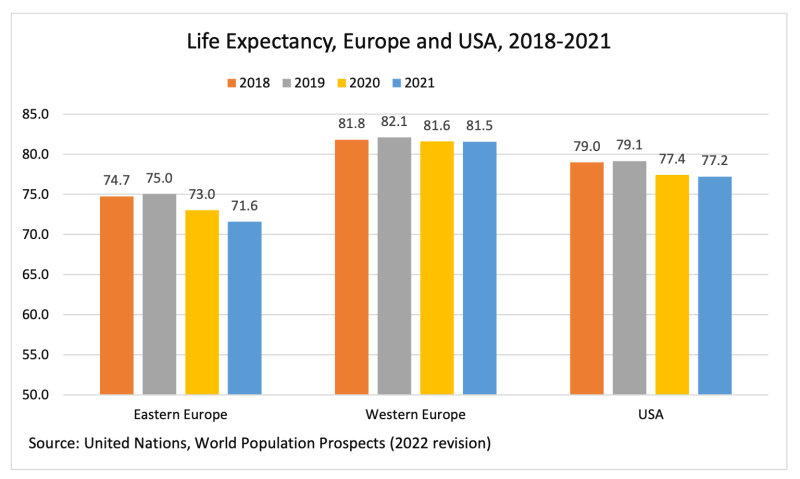
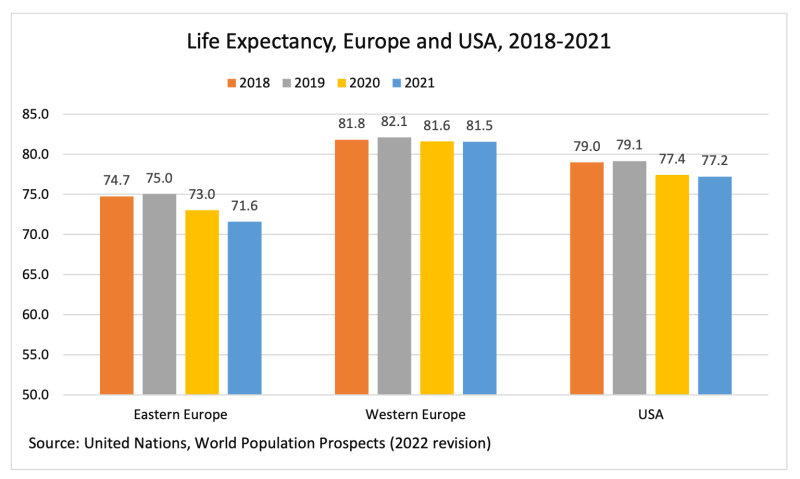
In the US, after the covid drop of 2020 which on its own should have led to a 2021 rebound, there was instead a further drop of 0.2 years. A drop also occurred in Europe in 2021, influenced heavily by the steep setback in Eastern Europe.
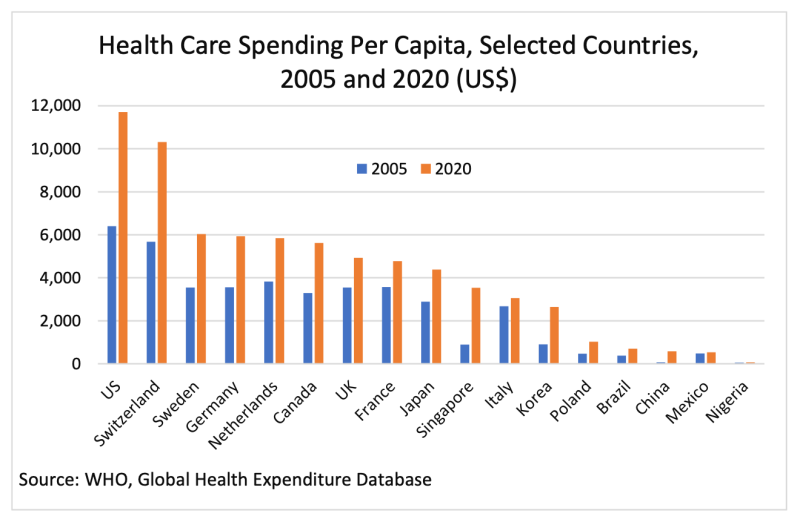
In terms of spending levels, in the 1960s it was normal for Western countries to spend about 4 percent of their GDP on things recognised as ‘health.’ Today, the comparable figure is nearly 20 percent for the US and 10 percent or more for the EU, increasing rapidly in recent years. Note particularly that China, with health costs per person about one-twentieth of those in the US, achieves a higher life expectancy.
On these figures alone, we can say without hyperbole that health is a policy disaster zone and has been so for a long time. Western countries have massively ramped up inputs without achieving commensurate outputs.
The US has spent about double on health relative to Western Europe for decades, and this has yielded health outcomes worse than China and several countries in Latin America (like Costa Rica) or Central Europe whose health systems are easily 90 percent cheaper. Even Western Europe has spent far more on its health than should have been needed in order to achieve the outcomes it has seen, based on a casual reading of international health systems.
Of the many weird excuses offered in policy land for these basic numbers, let us suffice with swatting away two prevalent ones.
First, it is not the case that population aging is worse in the US than places like China or Eastern Europe. In fact it is the opposite. Second, it is not true that the US or EU is buying quality of life, as opposed to length of life, for its health dollars (see, illustratively, the worsening happiness reported on the US General Social Survey since 1972).
If not delivering length or quality of life, then what exactly has ‘public health’ been all about? We give a short, stylised answer to this question below, including a sense of what has been useful and what has not.
The Ups and Downs of Public Health Interventions Since 1800
The graph below shows changes in life expectancy over the past 200 years. Life expectancy in Europe and the Americas before 1850 was below 40, and everywhere else below 30.
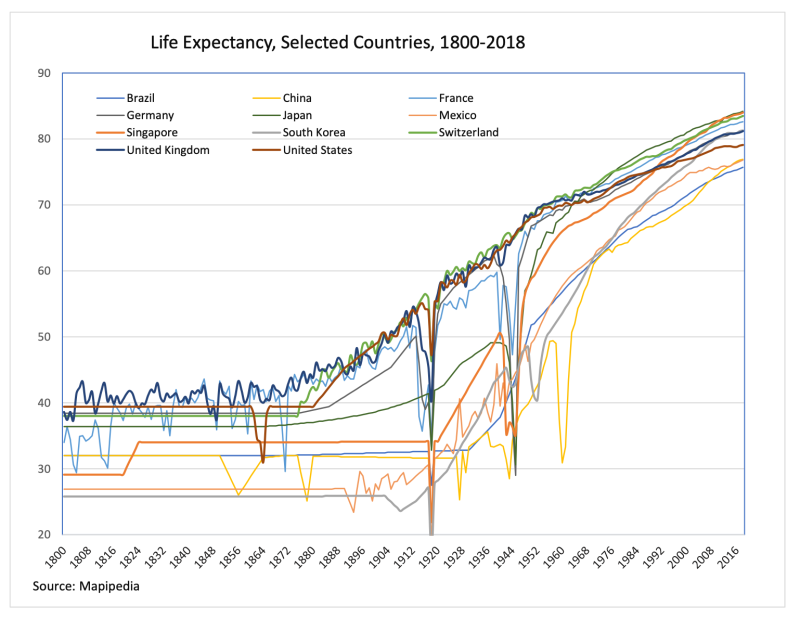
What changed was that great advances were made in public hygiene and sanitation, spearheaded by the Sanitarians and exemplified by the first Public Health Act in 1848 in the UK. The central focus of the Act was on cleaning up. In the ensuing decades the UK got underground sewage systems, clean water, running toilets, more food, and garbage collection. The promotion of basic hygiene and food security was the priority because these were the things that truly made a huge difference to people’s health.
As an aside, the Act also abolished the practice of quarantining that became so popular again during the covid era. A study published in 1951 noted that “in 1848 even the Royal College of Physicians admitted the uselessness of quarantine.” In the run-up to the 1848 Act, even contributors to the journal that became such a monument to anti-science during covid, the Lancet, were dismissing quarantining as either ignorant or despotic or both.
Switching from wood-fired indoor cooking with poor ventilation to gas cooking and then electric cooking with good ventilation also made a huge difference, in particular by reducing childhood mortality. To this day, in developing countries where cooking with solid fuels is still normal, studies show a drastic impact of this practice on child health and mortality.
Also relevant were a few key breakthroughs in medicine. Antibiotics, vaccines against rubella and smallpox, aspirin, other blood thinners, vitamin D, and a few other cheap medicines made a major difference when they arrived on the scene. Before 2020, when the WHO was still useful, it brought out a list of essential medicines to help poor countries determine which cheap medicines to purchase. After 2021 that list became corrupted with the addition of covid vaccines, just as the WHO itself became corrupted and is best regarded now as an anti-health organisation.
The importance of cheap interventions is also exemplified in the huge effectiveness of what are called GPs (general practitioners) in the UK and family physicians in many other countries. A study examining the rollout of family physicians in Turkey in the first decade of the 2000s concluded that “each family physician saves about 0.15, 0.46, and 0.005 lives among infants, the elderly, and children aged 1-4 per province every year.” Family physicians do the grunt stuff in health: helping with deliveries of babies, fixing up minor injuries, dispensing cheap and effective medicines, giving some inoculations, providing general healthy lifestyle advice, and so on.
What is perhaps surprising, but very important if one cares about optimising health spending, is how almost completely unimportant all the expensive stuff is for health. Major hospital operations, ICUs, designer medicines and so on basically do not move the dial, for three big reasons that medics often do not like to talk about.
The first is that hospitals are unhealthy places where visitors run major risks of getting sicker rather than getting better. The WHO, when it was still being useful, advertised studies that estimated that some 15 percent of people going to hospital pick up a nasty bug there, because after all it is where seriously sick people (including those sick with nasty bugs) go. That is a high risk that is practically never mentioned in the cost-benefit studies pharmaceutical companies churn out when marketing their latest wares.
Second, lots of expensive medicines and operations are given to people who are very close to death and have multiple other ailments, so preventing them from dying of one thing often just postpones death by a few weeks. The upshot is that the end of life is made lonelier, more painful and more stressful, but extremely profitable to both the hospital and Big Pharma.
Again, this is practically always downplayed in commercial health studies via a few useful tricks, like insisting that both treatment and placebo group have no other ailment than the one being studied and are thus much healthier than is true in practice.
Another trick is to compare an expensive new drug with an expensive old drug, and both only on fairly healthy populations rather than the sick ones who are more frequent drug recipients in practice. Much of the health system profits from the fear of death, with in-built massive exaggeration of benefits and underestimation of costs in the medical studies that routinely pop up in the Big Pharma advertising magazines (like the Lancet, the British Medical Journal, and so on).
A third reason why expensive interventions don’t move the dial much is that many of the medicines and operations pushed by Pharma and medics don’t actually work. For example, only 50% of drugs that get preliminary access to the US markets (after passing Phase II of that process) make it to full access (Phase III), with even fewer getting full approval, though they still make money for their manufacturers and distributors while being in ‘pending’ purgatory.
Also, tellingly, the large literature on ‘supply-induced demand’ (a booming line of research in the 1990s that has become a trickle in the top journals over the last 10 years) includes studies in which members of a doctor’s family were found to have received fewer operations on average than non-family individuals advised by the same doctor.
By implication, both the industry and the doctors themselves know that the benefits of their expensive interventions are exaggerated.
Today’s ‘new medicine’ exploits the credence-good problem that permeates health care. A credence good is a good whose quality and usefulness to you is unknown to you, but better known by ‘an expert’ on the supply side. In a market for a credence good, even a private one, the incentives at play lead the expert to overcharge and overtreat the ignorant patient. Medical negligence and liability laws only make this problem worse, as they lead to massive overtesting which in turn leads to mountains of false-positive diagnoses – fodder in turn for another lucrative racket.
The situation has become so bad and so distorted that by now the presumption of a wise observer is that most hospital visits worsen health and most new drugs cost far more than they are worth. Hospitals should now mainly be seen as fear-exploitation centres, with a few good doctors and nurses doing their best despite the perversity of their institutions.
Optimal Public Health
Exceptions prove the rule, and exceptions exist to the rule that ‘new medicine’ has little to offer. We do not deny the life-saving quality of an open-heart operation to replace a bulging section of the aorta of an otherwise healthy 77-year-old man expected to go on to live another 15 years. If such an operation costs less than the expected benefit in terms of quality life-years saved, an argument exists to fund it, whether publicly or privately.
Yet given the good aggregate health outcomes seen in Eastern Europe, China, and Latin America achieved on comparatively minute health budgets, and the economic and political considerations reviewed above, we conclude that a rather startling overall policy orientation is optimal.
The goal should be to set things up so as to offer more basic essential medicines and family physicians to the whole population, while simultaneously closing down most existing hospitals, health charities, pharmaceutical companies, and private clinics. Institutions that merely profit from death rather than averting it, while also failing to add quality to life, should have no reason to exist in a market where outcomes, rather than marketing slogans and virtue-signalling, are what matter.
Only those health services that are highly cost-effective relative to cheap prevalent alternatives (rather than relative to other expensive medicines, as most new health products get judged currently) should then be reallowed onto the market. The starting presumption of an optimal health system should be against any claim of effectiveness. ‘Ineffective until proven otherwise’ should be the mantra applied to all expensive interventions, and this proof should be verified by independent, randomly selected scientists comparing the results of every new offering against the results available from pre-existing, cheap medicines and interventions, in samples representative of the population of people who would be likely to take the new offering.
Following this logic, we advocate closing down about 80 percent of the health sector, leaving only the most useful bits. A grandfathering period of a few years to complete the close-down, in which no new ‘health’ organisations can enter the market, would prevent a quick reentry of the same villains. The presumption of low efficacy of any new medicine or intervention should also help to prevent new tragedies akin to the opioid crisis, or other health emergencies directly caused by fancy drugs.
The notion of what public health is about should also change. Clean water, cooking on electricity or gas, low air-polluting industries, efficient garbage collection, underground sewage, and encouragement towards healthy dietary habits and participation in sport should all be considered core public health investments. With the vast amount of money freed up by abolishing the useless bits of their present health spending, the US and other Western governments can easily afford large upgrades in these areas.
We should also consider the health benefit to the world as a whole of migration, a benefit that was forgotten and turned on its head during covid. Sunetra Gupta nicely argues that the world population becomes healthier with international travellers collecting and disseminating weak variants of viruses, thereby immunising populations against strong variants very much as vaccines do, but far more cheaply and more effectively. Exposure to travellers gives the immune system a good workout: enough to get stronger, not too much to succumb.
Beyond advocating healthy eating, exercise, and robust international travel, there is the question of what role optimal public health policy has in promoting particular lifestyles. At present, the West is burdened with high and increasing levels of obesity, gaming addiction, mental health problems, and loneliness.
To the health industry all this is a boon, providing a steady stream of victims to fleece. What is needed to overcome these tragic problems, in our opinion, is primarily a revival of healthier social systems whose decay was a primary agent in creating them. We advocate for communities that are more functional in general, and that look after the young and the lonely by slotting them into productive roles rather than treating them as victims.
On balance, both public and private health bureaucracies stand in the way of this type of community revival, because functional communities are rivals for the same resources and the same ‘clients’ as health bureaucracies.
We expect therefore that closing down much of our current health system would help to revive communities that would then start to tackle those of our modern health problems that are largely social in origin. The same goes for many mental health ‘special needs:’ the health industry that benefits from giving large fractions of the population a lucrative label (autistic, borderline, trans, bipolar, ADHD, OCD, and so on) should be closed down and their prior activities declared criminal profiteering, leaving it to reviving communities to decide whether and when such labels are useful, and ultimately to help individuals with different talents and proclivities find ways to contribute.
Getting Real
We fully recognise that our analysis above is unpalatable politically and indeed that there is no trigger in practice for what we propose to happen, at least in the short run. After all, we are advocating closing down about a sixth of the US economy and over 10 percent of the EU economy. Parasitical entities of that size do not let go of their victims without a fight. They will push all kinds of magical and technical ‘remedies’ for the many ills ailing people and will demonise through all means available anyone who advocates for their demise.
We expect that the vast majority of even those doctors and health professionals in the anti-lockdown movement will be against our proposals, for the simple reason that many of them would not have a job in our preferred solution. We have spoken to several high-profile professors of medicine and practicing specialists who see all the ills we see, but who still hang on to some magical technical solution that will sort it all out. They dream of perfect measures of health and health needs to feed into a benevolent health bureaucracy. They want to get rid of a few managers, but only to take their place and expand the health system.
Our much cheaper and simpler solution is to go back to health basics, close down most of the sprawling health sector, and build back only what works.
Join the conversation:


Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.