The following excerpt from my book, The New Abnormal, was published by the Daily Wire last week and reprinted here with permission. Enjoy…
Shortly after I published the Wall Street Journal piece arguing that university vaccine mandates were unethical, the University of California, my employer, promulgated its vaccine mandate. I decided then it was time to put a stake in the ground: I filed a lawsuit in federal court challenging the constitutionality of the university’s vaccine mandate on behalf of COVID-recovered individuals. It was already clear from many robust studies that natural immunity following infection was superior to vaccine-mediated immunity in terms of efficacy and duration of immunity.
At the time I was an unlikely candidate to challenge the prevailing vaccination policies. I was deeply embedded in the academic medical establishment, where I had spent my entire career. In my capacity as a psychiatric consultant on the medical wards and in the emergency department, I had suited up in PPE (personal protective equipment) to see hundreds of hospitalized COVID patients, witnessing the worst that this illness can do. Nobody needed to explain to me how bad this virus could be for some individuals, especially the elderly with co-occurring medical conditions who were at significant risk of bad outcomes when infected.
I contracted the virus in July 2020, and despite my efforts to self-isolate, passed it to my wife and five children. Living and breathing COVID for a year, I eagerly awaited a safe and effective vaccine for those that were still not immune to this virus. I happily served on the Orange County COVID-19 Vaccine Task Force, and I advocated in the Los Angeles Times that the elderly and sick be prioritized for vaccination, and that the poor, disabled, and underserved be given ready access to vaccines.
I had worked every day for over a year to develop and advance the university’s and state’s pandemic mitigation measures. But as the prevailing COVID policies unfolded, I became increasingly concerned, and eventually disillusioned. Our one-size-fits-all coercive mandates failed to take account of individualized risks and benefits, particularly age-stratified risks, which are central to the practice of good medicine. We ignored foundational principles of public health, like transparency and the health of the entire population. With little resistance we abandoned foundational ethical principles.
Among the most glaring failures of our response to COVID was the refusal to acknowledge the natural immunity of COVID-recovered patients in our mitigation strategies, herd-immunity estimates, and vaccine-rollout plans. The CDC estimated that by May 2021, more than 120 million Americans (36 percent) had been infected with COVID. Following the Delta-variant wave later that year, many epidemiologists estimated the number was close to half of all Americans. By the end of the Omicron wave in early 2022, that number was north of 70 percent. The good news — almost never mentioned — was that those with previous infection had more durable and longer-lasting immunity than the vaccinated. Yet the focus remained exclusively on vaccines.
As I argued in a coauthored article, medical exemptions for most vaccine mandates were too narrowly tailored, constraining physicians’ discretionary judgment and seriously compromising individualized patient care. Most mandates only allowed medical exemptions for conditions included on the CDC’s list of contraindications to the vaccines — a list that was never meant to be comprehensive. CDC recommendations should never have been taken as sound medical advice applicable to every patient.
Further exacerbating this problem, on August 17, 2021, all licensed physicians in California received a notification from the state medical board with the heading “Inappropriate Exemptions May Subject Physicians to Discipline.” Physicians were informed that any doctor granting an inappropriate mask exemption or other COVID-related exemptions “may be subjecting their license to disciplinary action.” In what was perhaps a deliberate omission, the “standard of care” criteria for vaccine exemptions was never defined by the medical board. In my eighteen years as a licensed physician, I had never previously received any such notice, nor had my colleagues.
The effect was chilling: since physicians naturally interpreted “other exemptions” to include vaccines, it became de facto impossible to find a doctor in California willing to write a medical exemption, even if the patient had a legitimate contraindication to the COVID vaccines. One of my patients was told by his rheumatologist he should not get the COVID vaccine, since he was at low risk from COVID and in this physician’s judgment his autoimmune condition elevated his risks of vaccine adverse effects.
This patient, who was subjected to a vaccine mandate at work, immediately asked this same physician for a medical exemption. The doctor replied, “I’m sorry, I cannot write you an exemption because I’m afraid I might lose my license.” I heard many stories of similar egregious violations of medical ethics under these repressive mandates and the enforcement regime that bolstered them.
As the vaccines rolled out in 2021, I spoke to many students, faculty, residents, staff, and patients who were aware of these basic immunological facts and were asking legitimate questions about vaccine mandates. Many correctly saw no medical or public health justification for subjecting themselves to the risks of the novel vaccines when they already had superior natural immunity. Others had moral concerns but did not qualify for a religious exemption, because religion was not central to their conscience-based objections.
They felt intimidated, disempowered, and vulnerable in the face of immense pressure to go along. Many physicians and nurses were afraid to speak up in the climate of coercion. Public health officials ignored inconvenient scientific findings, suppressed reasonable questions, and bullied into silence any skeptical physicians or scientists. Institutions promulgating mandates stigmatized and punished those who refused to comply. I had never seen anything like this in medicine.
Why did I file a lawsuit in federal court against my own employer? I had nothing to gain personally by this and a lot to lose professionally. I decided I could not stand by and watch the ethical disaster unfold around me without attempting to do something. In my position as Director of Medical Ethics at UCI, I had a duty to represent those whose voices were silenced and to insist upon the right of informed consent and informed refusal.
In the end, my decision to challenge these mandates came down to this question: How could I continue to call myself a medical ethicist if I failed to do what I was convinced was morally right under pressure? Projecting ahead to the required medical ethics course I taught to first and second-year medical students at the beginning of each year, I could not imagine lecturing on informed consent, moral courage, and our duty to protect patients from harm if I had failed to oppose these unjust and unscientific mandates. I simply would not have woken up each day with a clear conscience.
The university did not take kindly to my legal challenge, as you might imagine. Administrators allowed no grass to grow under their feet before responding to this dissident within the ranks. I had petitioned the court for a preliminary injunction to put the vaccine mandate on hold while the case was litigated in court. The judge declined this request, and the following day the university placed me on “investigatory leave” for alleged noncompliance with the vaccine mandate. Instead of waiting for the federal court to decide my case, the university immediately banned me from working on campus or working from home.
I was given no opportunity to contact my patients, students, residents, or colleagues and let them know I would suddenly disappear. An email from one of the deans, sent after I had left the office for the day, informed me that I could not return to campus the following day.
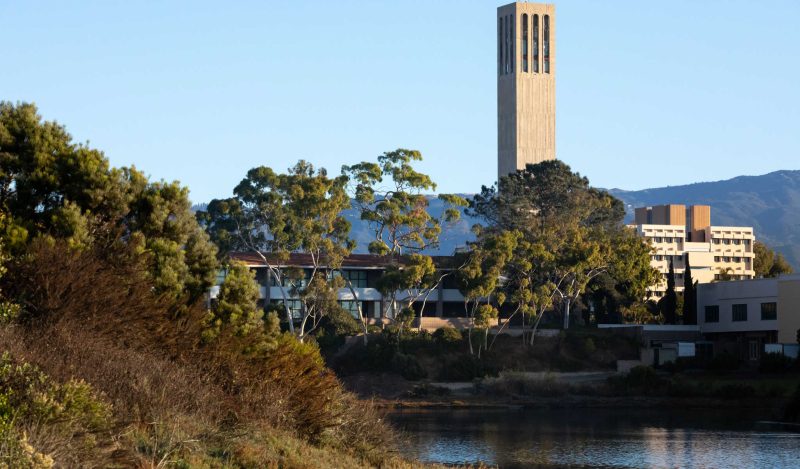
As I drove away from campus for the last time that day, I glanced at the sign on the corner near the hospital. The sign, which had been up for months, read in large block letters, HEROES WORK HERE.
Republished from the author’s Substack
Join the conversation:

Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.