[Full PDF of report is available below]
An Awkward Problem
The world of international public health is in a precarious position. Current policy, resources, personal careers, and the very credibility of major organizations are aligned with the recent statement from the World Health Organization (WHO) that:
Epidemics and pandemics of infectious diseases are occurring more often, and spreading faster and further than ever, in many different regions of the world.
Focus has shifted from the highest burden diseases, and the community-based empowerment required to tackle them, to preventing, identifying, and mitigating diseases that are rare and/or of relatively low burden, or even hypothetical. Namely, a new focus on sudden outbreaks of infectious disease or, in their more spectacular rendering, ‘pandemics.’
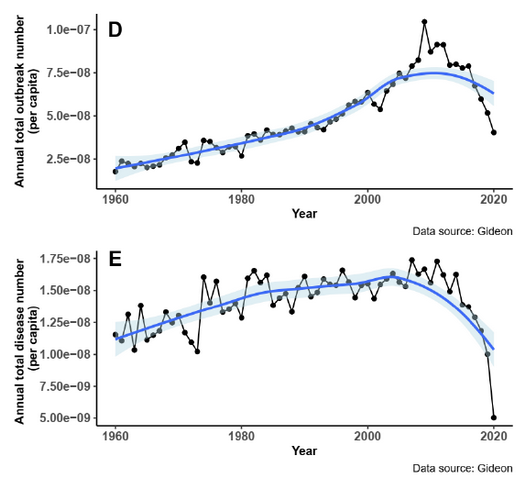
The challenge with this approach is that a thorough review of the evidence base underpinning the WHO’s agenda, and that of partners including the World Bank and G20, demonstrates that the above statement is inconsistent with available data. The largest database on which these agencies rely, the GIDEON database, actually shows quite a contrary trajectory. The burden of outbreaks, and therefore risk, is shown to be reducing. By implication, the largest investments in the history of international public health appear to be based on misunderstandings, misinterpretations, and misrepresentation of key evidence.
Weighing Truth and Opportunity
Public health policy must always address threats in context. Every intervention involves a trade-off in terms of financial, social, and clinical risk. The WHO defines health in terms of physical, mental, and social well-being, and an intervention in one of these areas can impact all three. This is why public health agencies must consider all aspects of direct cost, opportunity cost, and risk when formulating policy. It is why communities and individuals must have adequate information to make decisions in their own cultural, social, and ecological context.
To make sure policy assumptions and evidence is sufficient, it is therefore imperative to include broad information from multiple sources. Reliance on epithets, dogma, deplatforming, and censorship are therefore intrinsically dangerous. This is all, of course, meant to be coded into the normative principles of decolonization, human rights, and equity on which the WHO’s constitution is based.
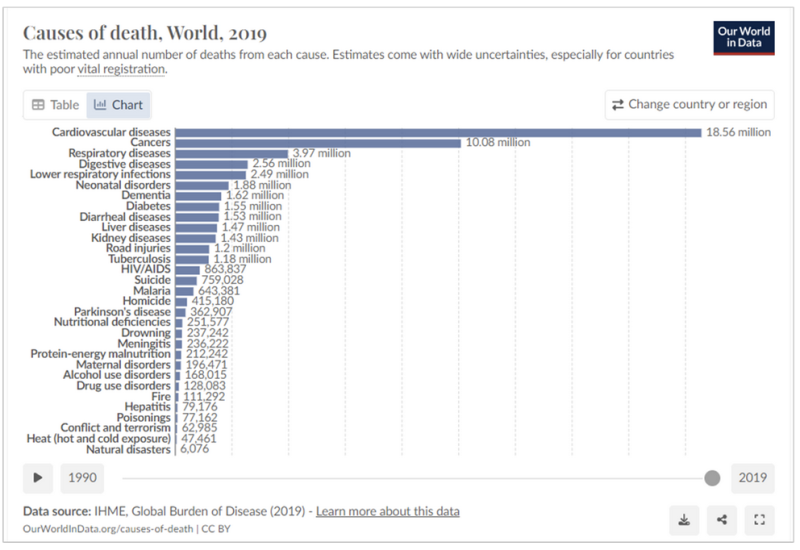
So, back to the precarious position in which the WHO and the international public health community find themselves. They have staked their reputation and political standing on being the center of a centralized approach to save the global populace from urgent, impending, and recurrent emergencies; an existential threat to humanity as the G20 tells us. An objective analysis reveals that these emergencies are rarely likely to reach a level that justifies the diversion of serious resources from endemic and chronic diseases that do actually maim and kill at scale (see chart below).
Admitting such a reality, after touting the inevitability of disaster so loudly, would risk career prospects, derision, and diminished ability to monetize the post-Covid moment. Yet, to ignore wider considerations in global public health and the evidence that informs those considerations would require abandonment of basic principles and ethics. A dilemma that calls for honesty, introspection, and strength.
What the Data Actually Shows
REPPARE’s analysis of the evidence behind the WHO, World Bank, and G20 documents promoting the pandemic preparedness agenda show that recorded outbreaks, both arising within human populations and as ‘spillover’ of pathogens from animals, have increased in the decades before the year 2000, with burden now declining (graphic below).
However, it is inevitable that reporting of such outbreaks will be influenced by changes in both the capacity and incentive to report. These include the development of, and increasing access to, major diagnostic platforms including PCR and point-of-care antigen and serology tests, as well as improvements in communication infrastructure. Fifty years ago, many pathogens now readily identifiable could simply not be detected, or the diseases they cause be distinguished from clinically similar conditions. It is remarkable that this would be overlooked or downplayed by major health agencies, but this is, unexpectedly, the case.
The development of improved diagnostic technologies not only impacts reporting rates but has obvious implications for understanding the term ‘emerging infectious disease’ (EID). This frequently used term suggests that new threats are constantly emerging, such as the Nipah virus outbreaks of the past 25 years. However, while some pathogens have newly entered human populations, such as new influenza variants, HIV and the SARS-1 virus, others such as Nipah virus were simply not detectable without recent technological advances as they cause non-specific illnesses. We are now better at finding them, which puts us immediately in a better, safer position.
Crucially, actual mortality from these acute outbreaks has remained low for a century in contrast to other current health burdens. The much-quoted analysis of Bernstein et al. (2022) suggesting millions of outbreak deaths per year includes pre-antibiotic era Spanish flu and the multi-decade HIV event, averaging it across today’s population size.
However, as their own dataset shows, nothing like the Spanish flu has occurred in terms of mortality in the past century. As most Spanish flu deaths were due to secondary infection, and we now have modern antibiotics, it also provides a poor model for future outbreaks. With HIV and influenza excluded, pre-Covid acute outbreak mortality underlying current pandemic messaging is under 30 thousand people, globally, over the past couple of decades. Tuberculosis alone kills over 3,500 per day.
Covid-19 has, of course, intervened. It fits with difficulty into the main pandemic narrative for a number of reasons. First, its origin remains controversial, but appears likely to involve non-natural influences. While laboratory escapes can and (inevitably) will occur, the surveillance and response being proposed here is targeted at outbreaks of natural origin. Second, Covid-19 mortality occurred mainly in the elderly with significant comorbidities, meaning actual impact on overall life expectancy was far less than the raw reported mortality figures suggest (this also complicates attribution). If considered of natural origin, it appears as an outlier rather than part of a trend in the datasets on which the WHO, the World Bank, and G20 rely.
Time to Pause, Think, and Employ Common Sense
The evidence, assessed objectively, paints a picture of an increasing ability to identify and report outbreaks up to the decade 2000 to 2010 (which explains increases in frequency), followed by a reduction in burden consistent with an increasing ability to successfully address these relatively low-burden events through current public health mechanisms (which explains a lowering trajectory in mortality). This fits well with what one would intuitively expect. Namely, modern technologies and improving health systems, medicines, and economies have improved pathogen detection and reduced illness. There is much to suggest that this trend will continue.
In this context, the analyses of the WHO, the World Bank, and the G20 are disappointing in terms of scholarship and balance. A critic could reasonably suggest that a desire to address a perceived threat is driving a particularly gloomy analysis, rather than analysis objectively aiming to determine the extent of the threat. Such an approach seems unlikely to address the needs of public health.
To be clear, disease outbreaks harm people and shorten lives and must be addressed. And there are of course improvements that should and could be made to address this risk appropriately. In common with most aspects of medicine and science, this is best achieved on the basis of well-compiled evidence and scholarly analysis rather than allowing predetermined assumptions to drive outcomes.
By making claims contrary to the data, international health agencies are misleading governments of Member States down an unevidenced path with correspondingly high estimated cost and diverted political capital. This currently stands at $31.1 billion annually not including One Health measures and surge funding and at least 5 new global instruments; or about 10 times the WHO’s current annual budget. The urgency involved in the pandemic preparedness agenda is either contrary to evidence or poorly supported by it.
In view of their influence, international health agencies have a particular responsibility to ensure their policies are well-grounded in data and objective analysis. Moreover, governments have a responsibility to take the time, and effort, to ensure that their populations are well-served. It is hoped that the evaluation in the REPPARE report Rational Policy Over Panic presented with this article will contribute to this effort.
REPPARE, 12 February 2024. David Bell, Garrett Brown, Blagovesta Tacheva, Jean von Agris.
Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.