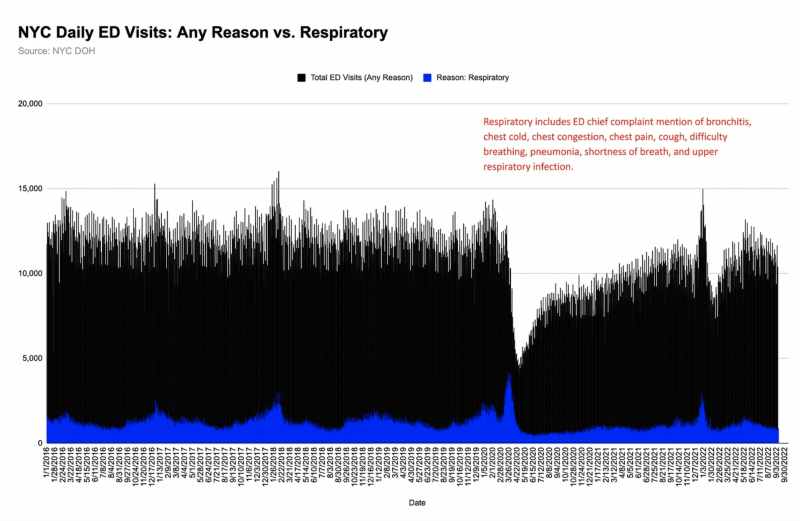
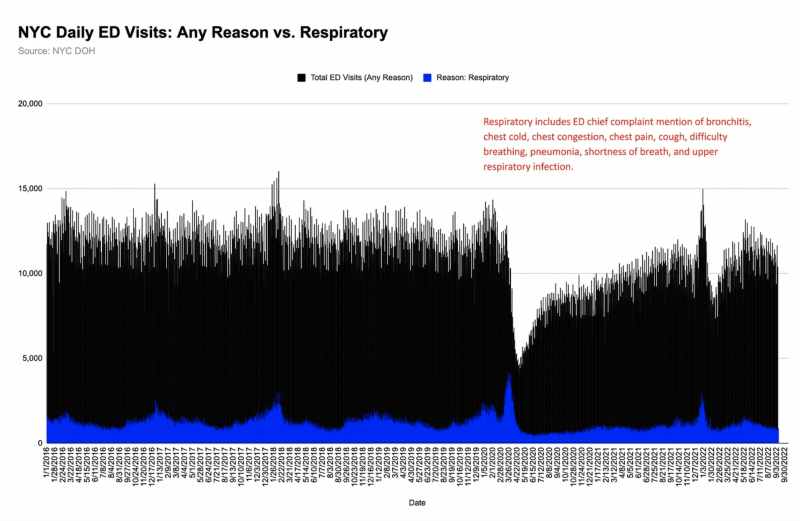
A few weeks ago, I posted data showing New York City’s hospital emergency departments were not at a breaking point in spring 2020. In fact, they were relatively empty and saw a 50% drop in visits.
I recently requested and obtained more files from the city’s health department to analyze alongside already-public data. (Raw data file with links to sources is at end of post.)
Here are five observations, with supporting graphs or tables.
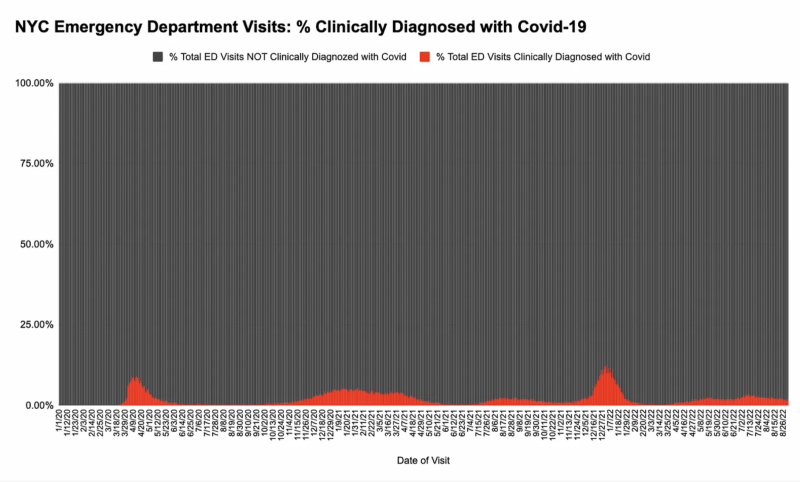
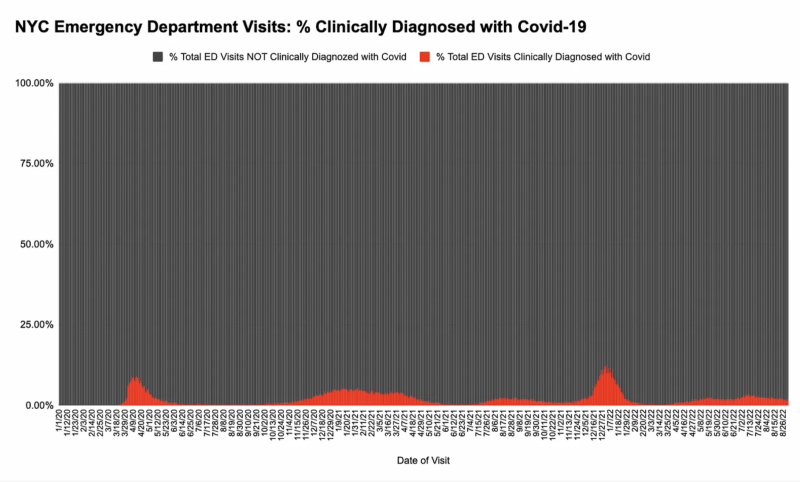
Observation One: NYC Emergency Departments weren’t overrun by people with covid-19.
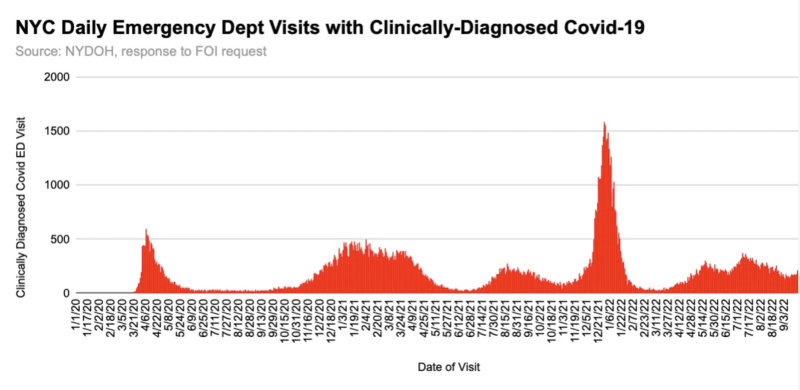
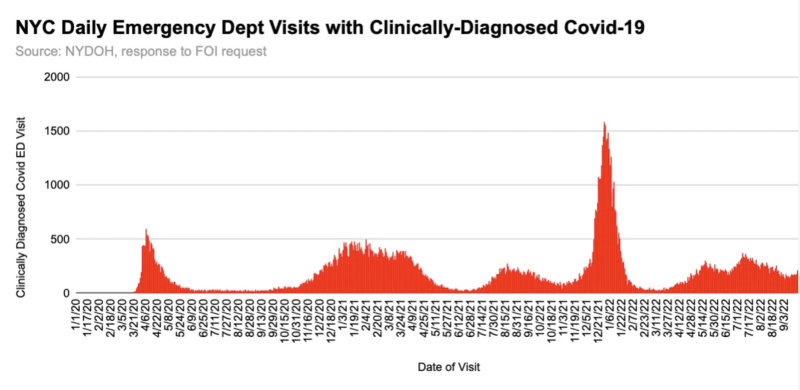
Only 3% of the people who came to New York City hospital EDs during the spring 2020 March – May wave were clinically diagnosed* with the virus. At no point did the percentage of visits to NYC hospital EDs with a covid diagnosis exceed 10%.
*Per NYC Dept of Health, a clinically-diagnosed covid ED visit is “a visit with an ICD-10 discharge diagnosis code of U07.1 or a SNOMED code of 840539006.” A clinical diagnosis does not have to include a laboratory-confirmed test for SARS-CoV-2, but a positive test irrespective of symptoms would receive diagnosis.
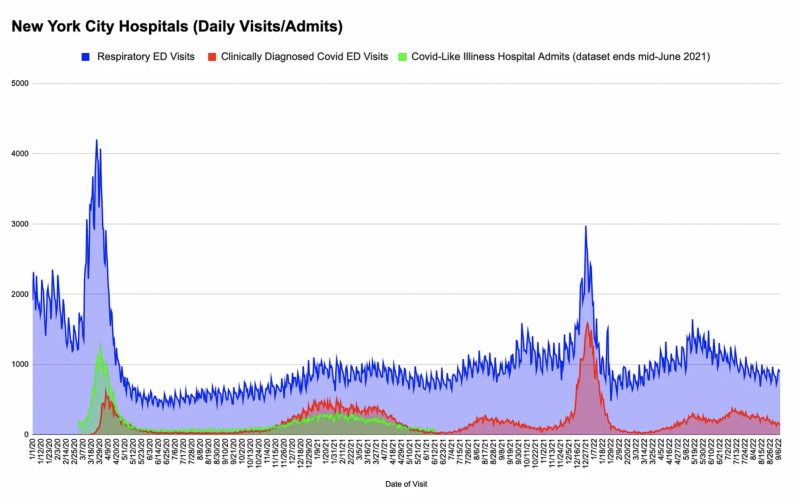
Covid-diagnosed visits were highest during winter 2022’s Omicron wave, when total daily ED visits briefly reached pre-pandemic respiratory-virus season levels, before again dropping below normal. We don’t know how many of these people had symptoms associated with the disease. We do know that the 2017-2018 flu season created busier emergency rooms for NYC than covid ever has.
Observation Two: NYC Emergency Room respiratory visit spike may have been panic-driven.
Respiratory visits for the 2019-2020 peaked in January, and were on the way down. New York Governor Cuomo issued a lockdown directive on March 10, 2020, and Calls to Emergency Medical Services soared, as did the number of people going to emergency rooms with respiratory symptoms.
But most emergency room visitors with respiratory symptoms were not diagnosed with covid. Huh.
To me, it appears the dramatic rise and fall was triggered by fear rather than “spread.”
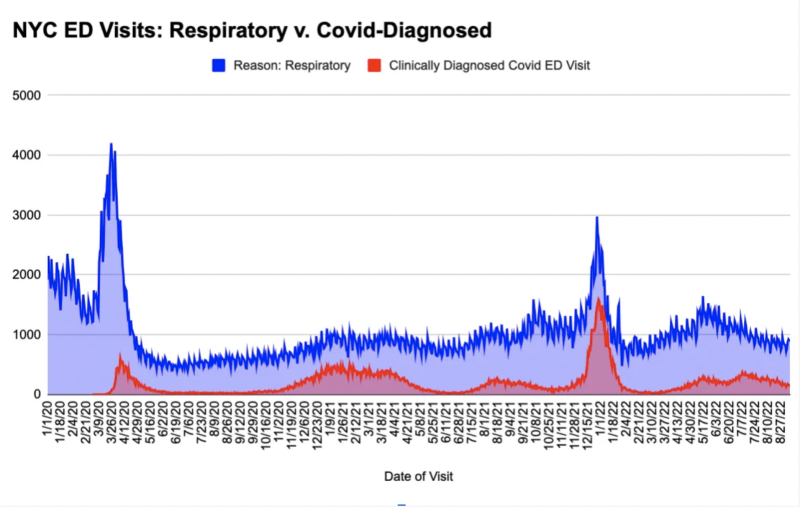
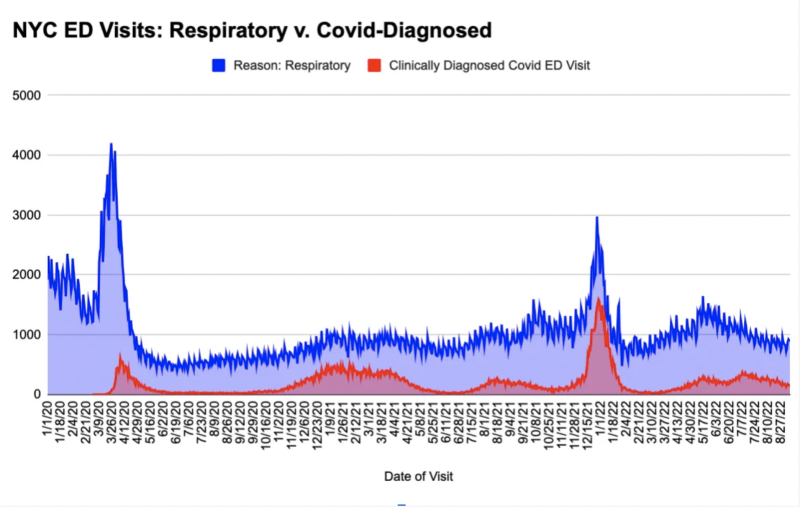
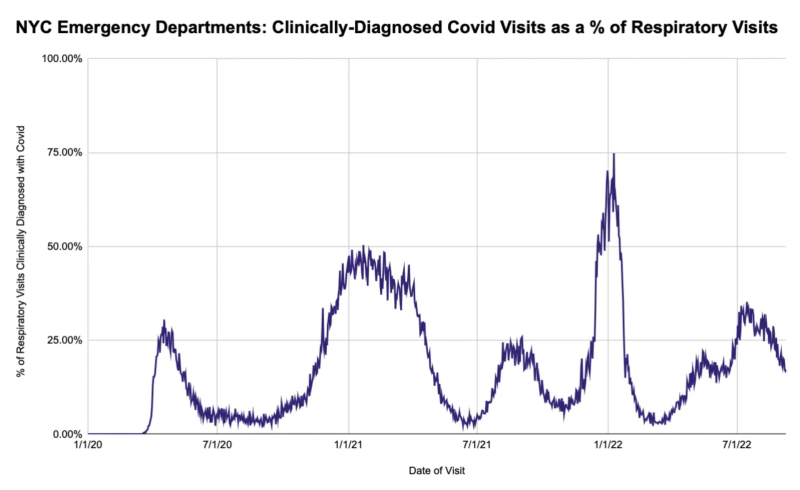
At spring 2020’s peak, the ratio of respiratory visits to covid diagnosis was 30%, which also points to at least some overreaction, psychogenic illness, or symptoms from non-covid causes.
Covid-testing in emergency rooms may have been lower in those early weeks, but a “diagnosis” doesn’t require testing.
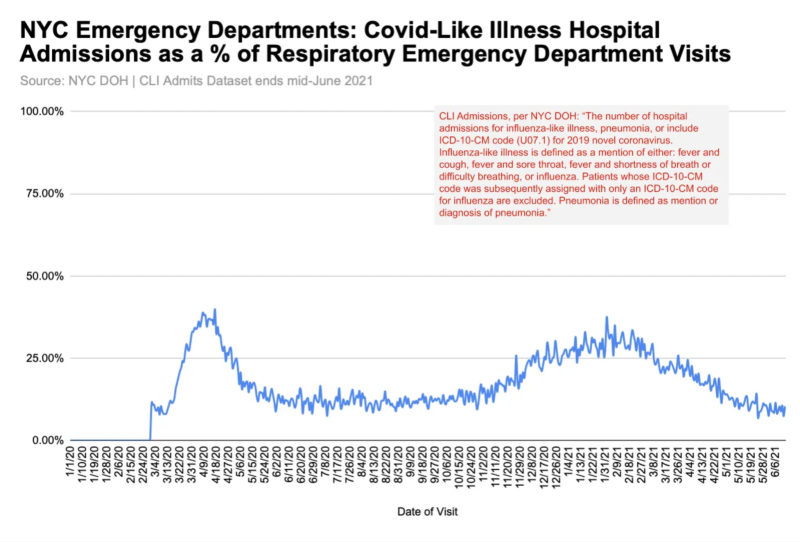
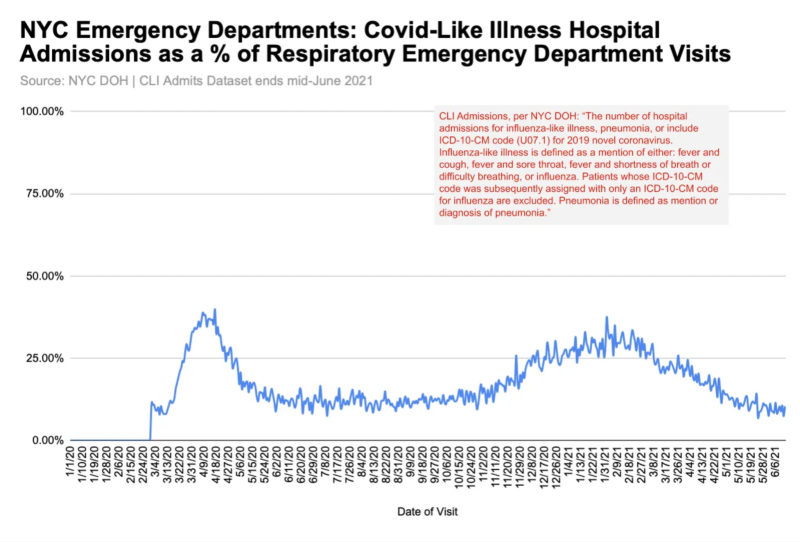
Observation 3: Most people who visited NYC emergency rooms between March 2020 and June 2021 for respiratory symptoms were not admitted to the hospital.
Peak hospital admissions for covid-like illness (CLI) were 40% of respiratory emergency department visits — another data point that hints at folks rushing to the ER at the first sign of a cough.
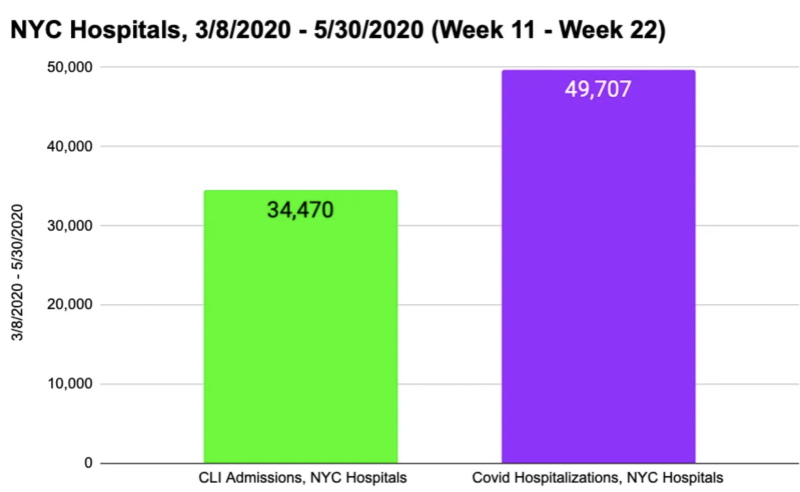
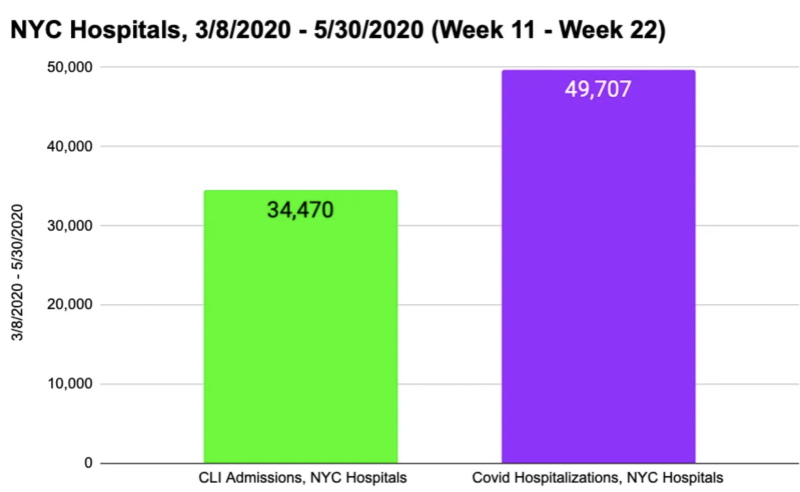
Observation 4: Many patients counted as covid hospitalizations in spring 2020 were not admitted with covid-like illness (CLI).
Data indicate that approximately 40% of inpatients with a covid diagnosis (via test, symptoms, or both) from mid-March through April 2020 had not been admitted with covid-like illness.
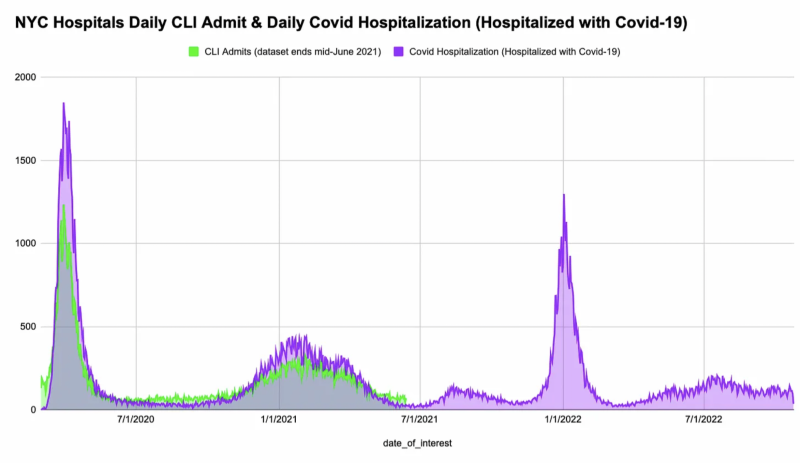
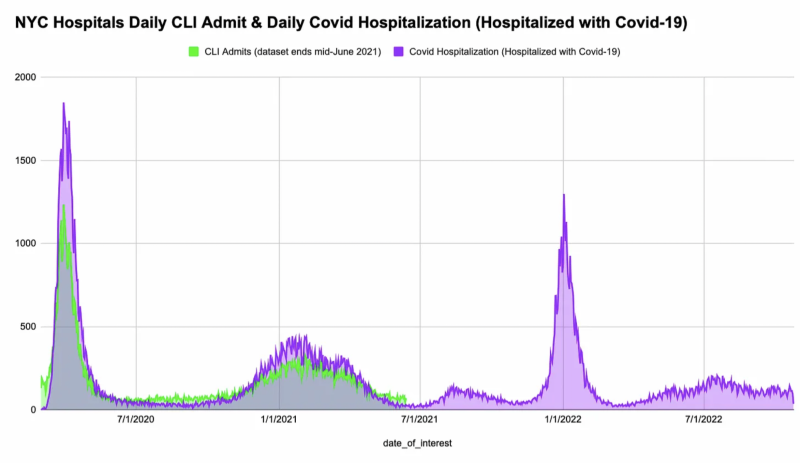
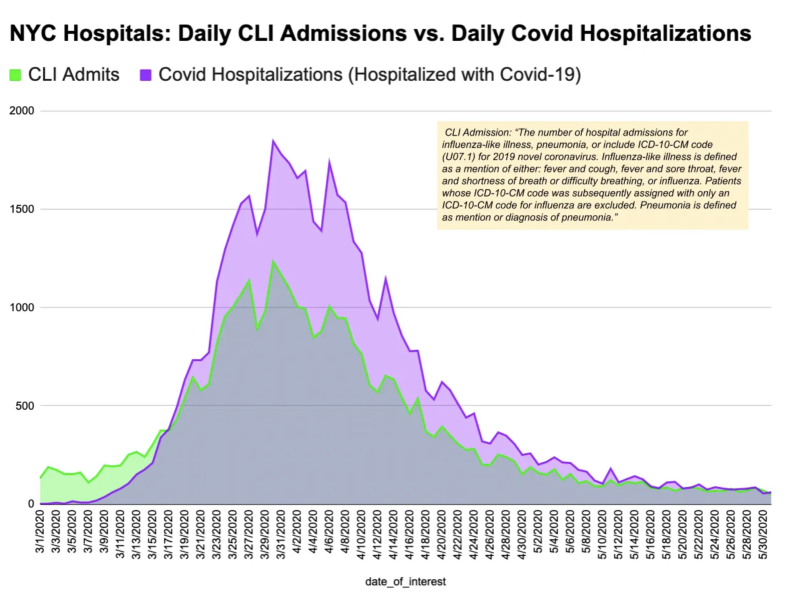
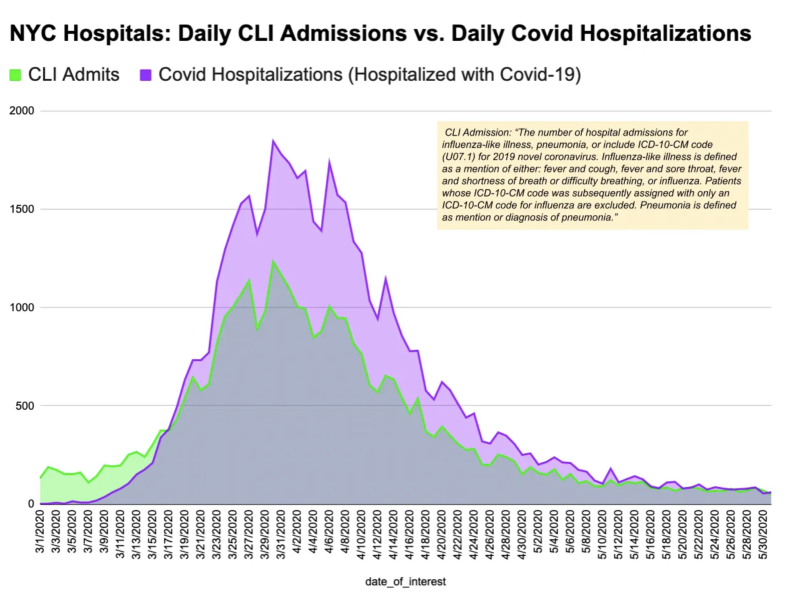
With such a broad definition of covid-like illness, there’s little chance hospitals *missed* coding people (including nursing home residents) who came to the hospital with symptoms that could have been caused by SARS-CoV-2. Patients admitted to the hospital for any reason were being tested for the virus – sometimes repeatedly.
While the “gap” between the two sets of numbers could point to nosocomial or attendant-borne spread, it could also simply be the result of incidental positives.
Observation 5: The relationship between hospital inpatient deaths with covid on the death certificate and people who were hospitalized because they had covid is unclear.
The gap between CLI admissions and covid hospitalizations (shown below) started seven days after the stay-home order. In the weeks that followed, it appears more people were being coded daily as covid hospitalizations than were being admitted to the hospital with CLI. From March 18th through May 30th, there were ~16,200 more covid+ hospitalizations than CLI admissions.
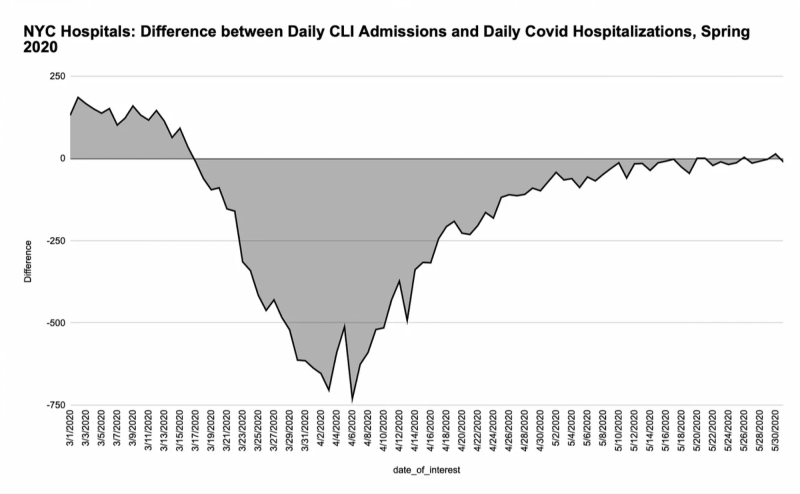
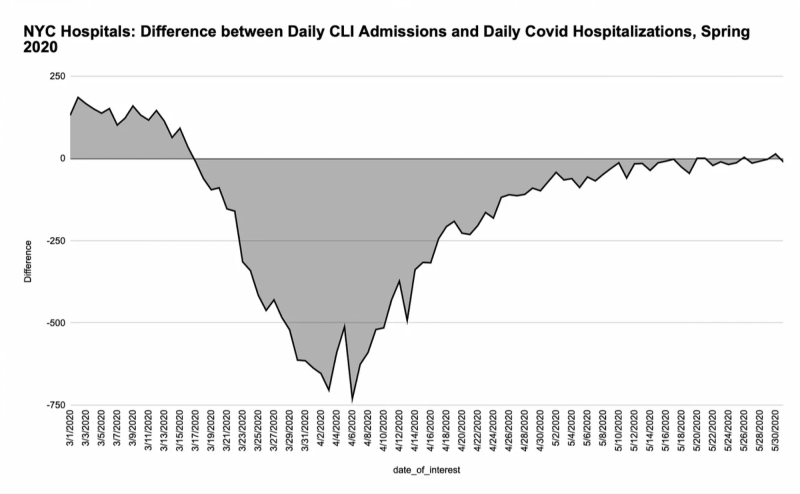
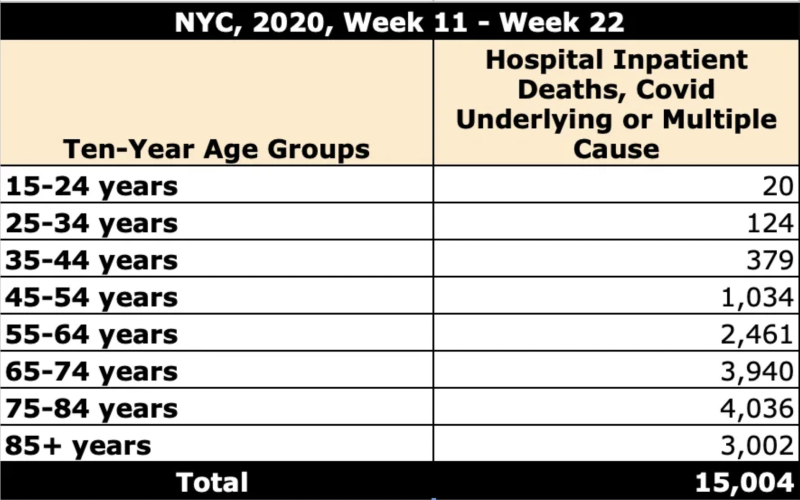
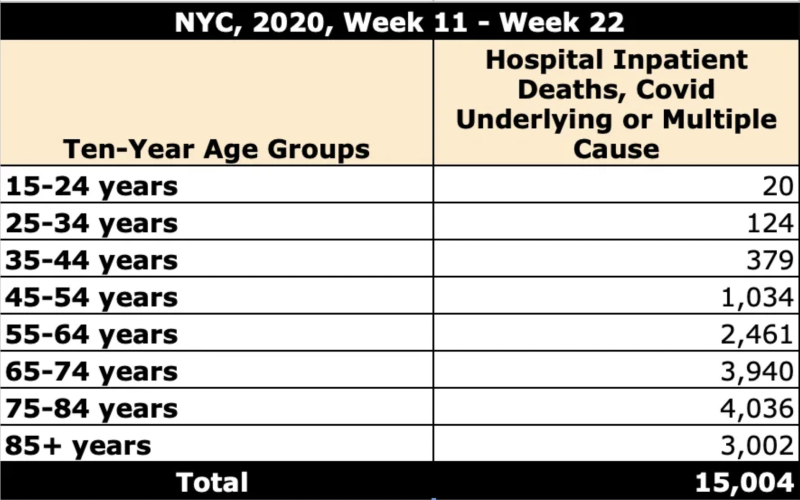
Over 15,000 NYC hospital inpatient deaths in these weeks have covid on the death certificate, per CDC WONDER. Without detailed record review, there’s no way of knowing how many of the 15K had covid symptoms when they were admitted.
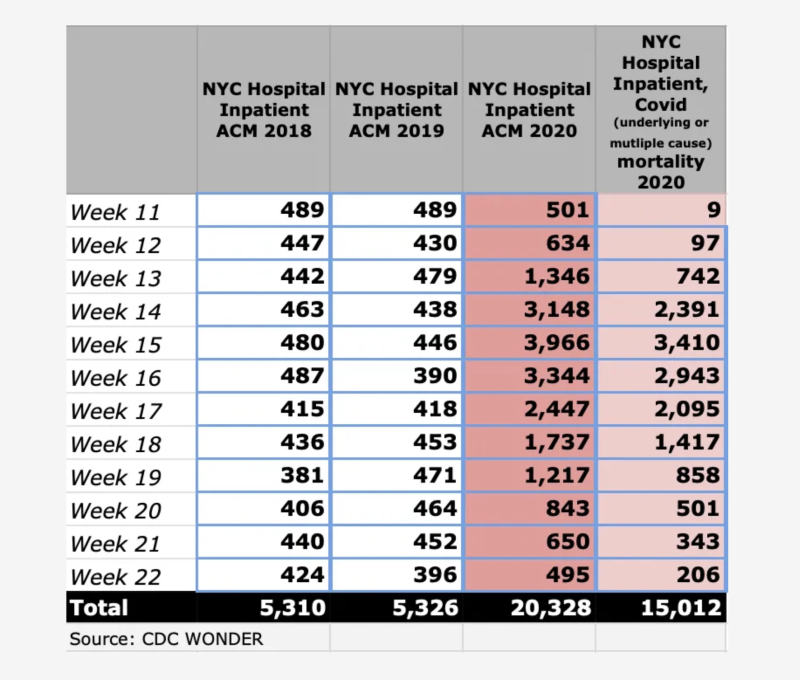
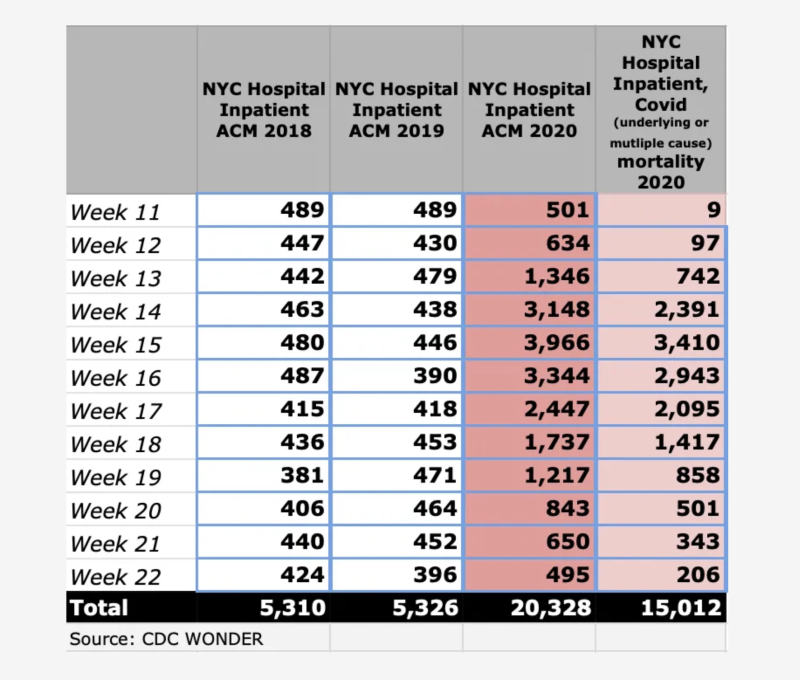
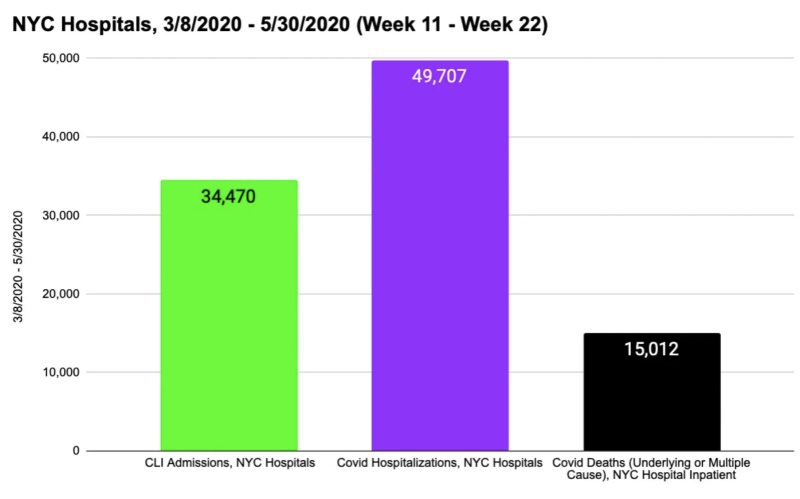
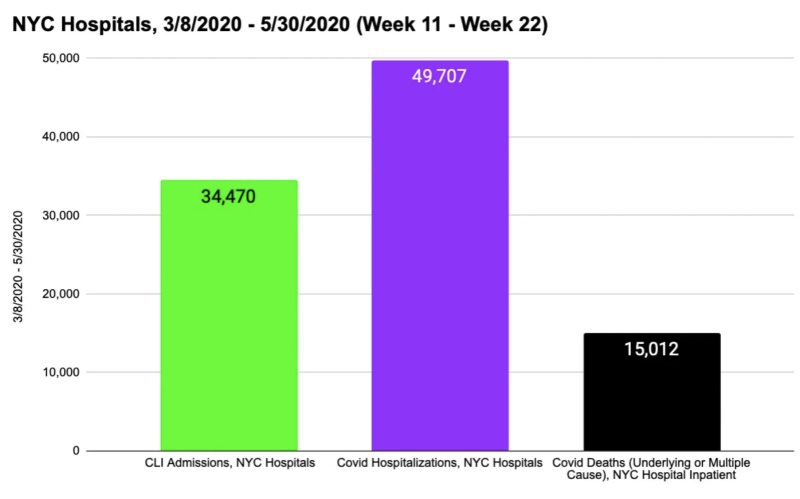
Covid-attributed deaths were 44% of CLI Admissions and 30% of covid hospitalizations. Must’ve been a lot of nursing home residents who were transferred to hospitals, right?
Not really. Only 13% (~2,000) of those 15K covid hospital deaths were from nursing homes.
New York’s a big city, but 13,000 covid hospital inpatient deaths in eleven weeks among people who were transfers from nursing homes defies credulity. We’d expect less-healthy, more vulnerable people to be hospitalized for and with covid, but these numbers and age distribution don’t mesh well with recent estimates of the pre-vax infection fatality ratio.
It’s no wonder Michael Senger, Ethical Skeptic, and other analysts (including me) have said it was misuse of ventilators, protocol-induced staffing shortages, isolation, failure to treat, similar factors that resulted in thousands of Spring 2020 iatrogenic deaths in New York City and elsewhere.
I welcome other insights, questions, and analysis related to the NYC 2020 mortality event. Other posts and data file for the current article below.
All Posts Related to New York City’s Spring 2020 Mortality Event
Republished from the author’s Substack
Join the conversation:


Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.









