We have heard a lot about health care worker vaccine mandates as the Supremes up held the federal CMS vaccine mandate. This mandate allows Centers for Medicare & Medicaid Services (CMS) to withhold Medicare funds from any healthcare provider organizations that do not implement a vaccination requirement across their workforce. The new deadline is February 28. By then the omicron surge may very well have passed. So, will or are the mandates helping?
President Biden’s statement on the heels of the Supremes’ decision:
“Today’s decision by the Supreme Court to uphold the requirement for healthcare workers will save lives: the lives of patients who seek care in medical facilities, as well as the lives of doctors, nurses and others who work there. It will cover 10.4 million health care workers at 76,000 medical facilities. We will enforce it.”
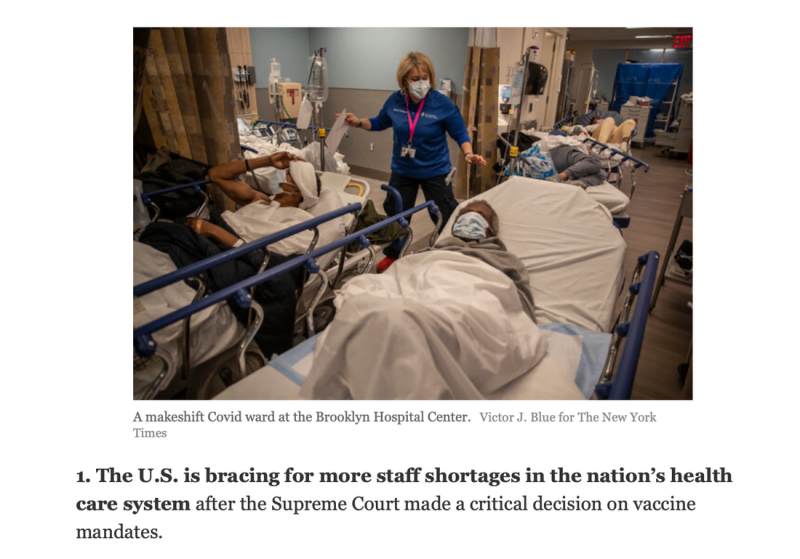
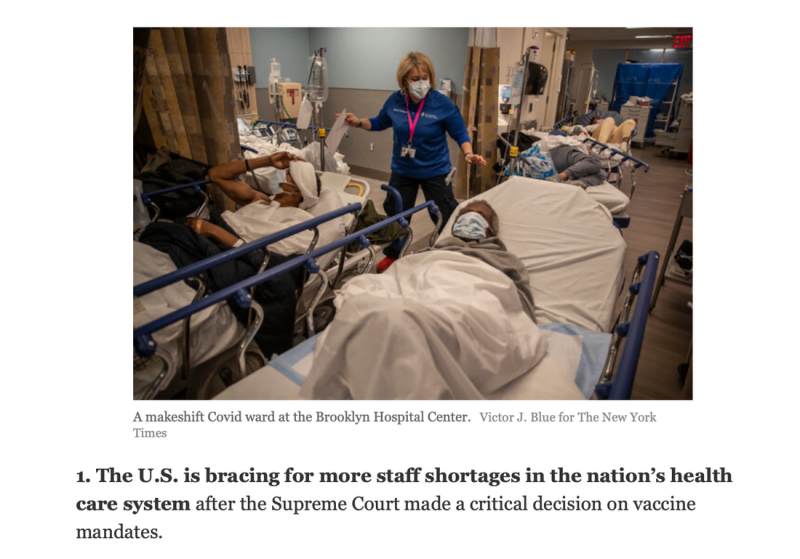
The New York Times loves to report on staffing shortages in hospitals. Real or fear? Mandate made or not?
Within states that have already implemented health care worker vaccination mandates the estimated loss of workforce is between 1-5%. This does not include those granted exemptions.
But the data from HHS shows:
States with >50% hospitals reporting critical staffing issues as of 1/11/2022:
New Mexico 53% (has HCW mandate)
Vermont 65% (has HCW mandate)
States with 30-49% critical staffing issues
North Dakota 35%
California 36% (has HCW mandate)
South Carolina 32%
Wisconsin 32% (has HCW mandate)
West Virginia 40%
Note: 4 of 7 (57%) states reporting critical staffing issues involving >30% of their hospitals have health care worker vaccination mandates in place.
States with current HCW mandates in place: California, Colorado, Connecticut, Delaware, Florida, Hawaii, Illinois, Maine, Maryland, Massachusetts, Michigan, Minnesota, Nevada, New Jersey, New Mexico, New York, North Carolina, Oregon, Pennsylvania, Rhode Island, Tennessee, Vermont, Virginia, Washington, and Wisconsin.
The “reasoning” behind health care worker vaccination mandates: infection prevention strategy in the healthcare setting coupled with a highly vaccinated workforce in order to substantially reduce the risk of transmission. Or: Keep the healthcare workforce working and robust.
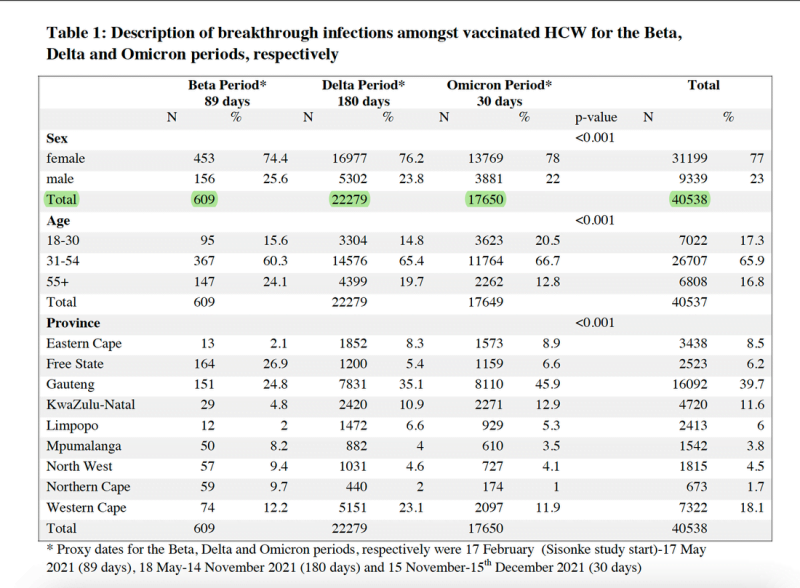
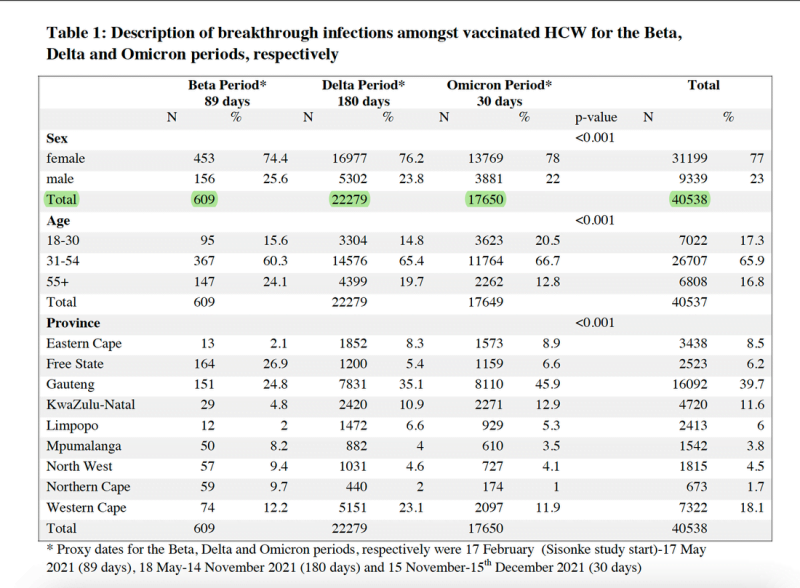
Does a vaccinated health care worker prevent transmission? Current data with the omicron variant does not support this. A recent pre-print study from South Africa looked at breakthrough case rates among HCWs during beta, delta, and omicron surges. This study is one of a series of clinical trials conducted by the Sisonke Group looking at the effectiveness of the Ad26.COV2.S COVID-19 vaccine (the JnJ vaccine) in preventing COVID 19 among HCWs. While it focuses on one vaccine and not on mRNA vaccines, it does give us insight into how breakthrough infections have increased among HCWs across variants from beta to delta to omicron as they became more transmissible and acquire more vaccine immune evasion. Note the omicron data was for just 30 days.
“We’re going to have a real challenge to the health-care delivery system — namely the number of beds, the number of ICU beds and even the number of health-care providers,” Dr Fauci recently said in an interview. “Even vaccinated people are getting breakthrough infections. So if you get enough nurses and doctors infected, they are going to temporarily be out of action. And if you get enough of them out of action, you could have a double stress on the health-care system.”
So, mandates to be vaccinated with “legacy vaccines” developed against the original Wuhan virus will help with that?
Well let’s look at the US healthcare system capacity as a whole. One good indicator is acute care hospital bed occupancy. Before the pandemic hospital staffing and bed capacity was held at an ideal percentage in order to maintain profitability. Hospitals are in many ways are like hotels and the hotel industry has studied the effect of occupancy on profitability pretty thoroughly.
“It turns out that for medium price range hotels, 75% occupancy is the most profitable rate whereas for high-end hotels, 85% occupancy is peak profitability. Many hospital executives talk about 85% being the ideal occupancy rate for a hospital.”
This statement is from the Medical Economics Hospital Medical Director Blog. So every midnight the hospital bean counters calculate bed capacity. On average before the pandemic bed capacity was 80-85%. That number fluctuated based upon time of year.
So, what occupancy or capacity are the hospitals currently reporting? HHS aggregates hospital data including bed capacity and occupancy for adult acute care hospital beds and ICU beds. They do the same for pediatrics but it is less robust data. HHS data includes numbers of admissions from all diagnoses and suspected and confirmed CV19 cases. The latest data dump was January 11, 2022 and can be accessed here where you can look up your own state’s hospital data.
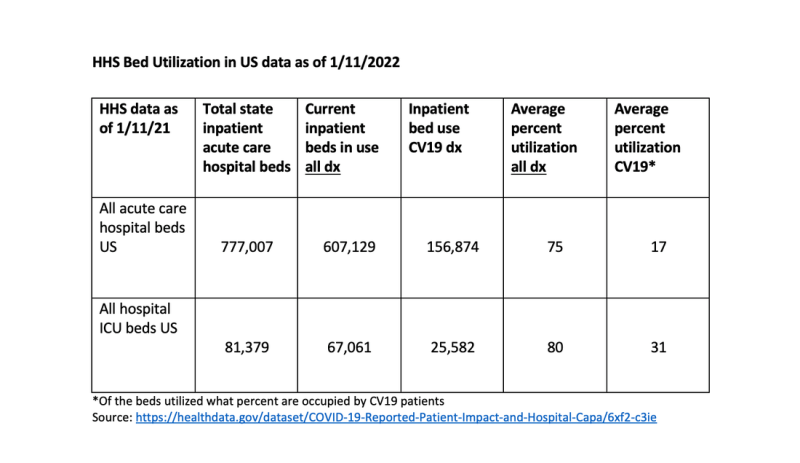
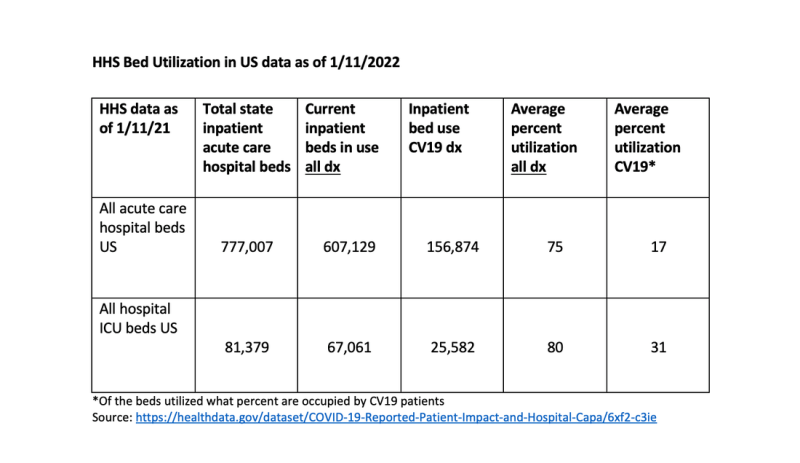
This data is aggregate adult data for the entire country calculated by pooling aggregate state data. Certainly, there will be states with higher bed utilization for all cause disease and CV19. Distribution of patients is not even especially in urban hospital centers where profits take precedent. Overall this national data does not appear as dire as the New York Times or Dr Fauci portend it to be.
Could that change? It is possible, but unless we are so metabolically different than other countries the rates of hospitalizations will be 40-60% lower with omicron.
To quote the FDA during it’s vaccine safety hearings: based upon the “totality of evidence” is it really beneficial to force health care workers to be vaccinated against a variant that the vaccine has very limited if any at all effect on reducing transmission or infection? In addition, of all people whose natural immunity needs recognition, it is health care workers.
Join the conversation:


Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.









