Experts are still warning darkly about a current surge in infections in some countries. But there has been a big change in the public mood across the world. Most people uncritically accept that governments did what they needed to do in previous years to ‘keep us safe,’ but at the same time lockdown and vaccination fatigue have set in and the driving force of public panic has subsided.
Democratic political leaders are at least adept at reading the signs and so are largely holding off for the time being.
Since the pandemic is perceived to be largely over, retrospectives and reviews have started to develop, some of which have been reported already. Fresh thinking is needed but is hard to find.
So how successful were government responses? Here we need to take our eyes off the trees and look at the wood, the big picture. There is no better way of doing this than surveying the chart of all-cause deaths over five years maintained by EUROMOMO, the European mortality monitoring service. Governments rapidly introduced harsh and extreme policies – is there any reason to believe they worked? Here is the chart for 28 November 2022:
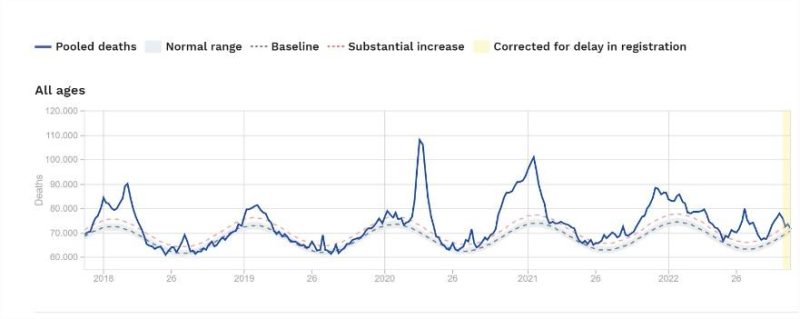
Overall, we see a trend of five declining peaks and progressively flattening curves, so the overall picture is one of gradual subsidence, which is only to be expected as immunity builds up.
From March 2020, governments in Europe and the Western world set out to ‘flatten the curve.’ Does that first curve look flattened to anyone? It is the sharpest and highest, occurring late in the traditional Northern winter season for respiratory viruses, and probably cut off quickly by the advent of summer.
Remember too that experts predicted disaster would ensue as governments started to remove restrictions going into summer. It didn’t happen. If there was no effect from removing restrictions, why should we believe there was any effect from imposing them?
The 2021 peak was a little lower, but the curve was somewhat wider, extending over a full winter season. Lockdowns were again the main weapon, especially in the first half of the season, and did not prevent a sharp rise before moderating somewhat before the peak.
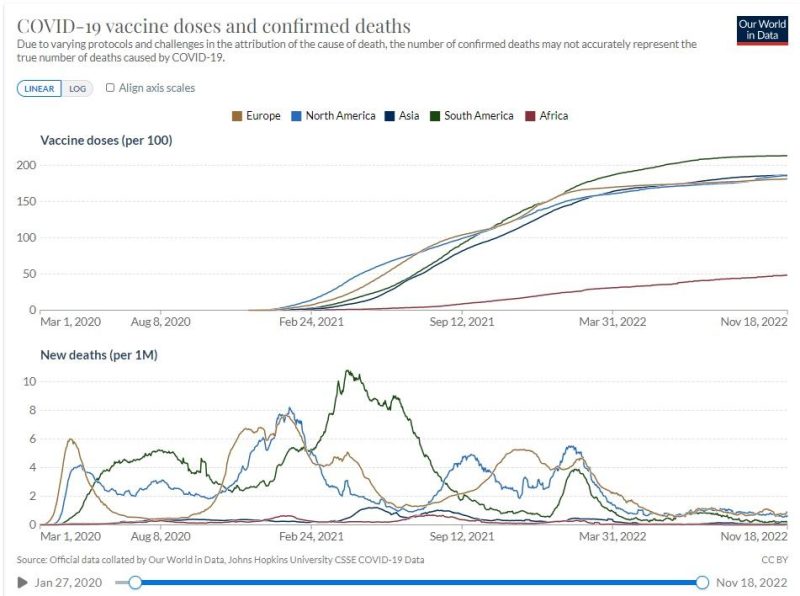
Vaccinations started building in the second half of the season and the increasing vaccination curve was inversely correlated with the declining mortality curve, but the mortality decline was almost identical with the previous year where there was no vaccination. According to Our World in Data, by 1 January 2022 12% of the European population had been infected and around 65% vaccinated, and the 2022 curve is the flattest.
A case can be made that the vaccination campaign contributed to the flatter 2022 curve as a component of ‘hybrid immunity;’ however we should also note the anomalous summer peak six months later, so it is by no means clear that the total outcome for the year was greatly improved.
The research evidence does not help much. There are certainly observational research studies showing that vaccination reduces COVID-19 positive mortality in particular windows of time. However, studies showing that it reduces all-cause mortality over more meaningful periods are very hard to find, starting with the celebrated randomized controlled trials, which are usually held to be the most high-grade evidence.
The defense against this line of argument is that vaccine trials do not have large enough trial populations to detect statistically significant differences in all-cause mortality. Maybe so, but several groups have aggregated the data from multiple trials. Benn et al. still found no improvement in all-cause mortality with the mRNA vaccines and, and Fraiman et al. also found the risk of serious adverse events was greater than the risk of hospitalization.
Turning to the observational trials, here is one of the elderly in Hungary, but it considers only the hospitalized population and has a broad exclusion period: participants were considered vaccinated only 14 days after receiving two doses of a vaccine and were followed up for 28 days thereafter.
If you died before or after that window of time or at home, you were not counted. Surely the whole point of assessing all-cause mortality is to assess total outcomes from the point of first receiving a vaccination. Otherwise, the effect on the pandemic curve is unknowable. See also the critique by Professor Norman Fenton and colleagues of the UK figures for this reason.
Another study of the elderly from Sweden excluded only the first seven days. The researchers slice and dice the data which highlights the extent to which outcomes are dependent on these analytical decisions, and find, inter alia, that vaccine effectiveness for mortality of a fourth dose for long-term care facility residents was only 27% between day 60 and day 126. Diminishing returns have set in, not only for infections but also for mortality.
A preprint analysis of Dutch municipalities by an independent researcher found: ‘We could not observe a mortality-reducing effect of vaccination in Dutch municipalities after vaccination and booster campaigns.’
A systematic review based on a selection of 42 studies found that the first dose of the Pfizer vaccine reduced relative risk for mortality against the B1.1.1 variant by 72% between day 14 and day 20, and by 0% against the B1.30 variant. Effectiveness was 100% at day 14 after the second vaccination. What happened next? What happened in the Age of Omicron?
These results are so limited and qualified, it is hard to see how policymakers could use them as a basis for policy decisions.
Other well-publicised studies rest on similarly weak foundations. These include: modeling again (predict exaggerated loss of life if no vaccination, and then argue that these virtual or hypothetical lives were saved by vaccination – see this critique on Brownstone); and differential analysis of small variations between a select group of peer countries. These differences disappear at the global level. All regions are converging on low COVID-19 mortality, including Africa with its low vaccination rates. Any correlation between vaccination and mortality cannot be seen at this level. And in any case, whatever happened to ‘correlation is not causation?’
COVID-19 has brought about the greatest surge in the research literature in living memory – it is not acceptable that we have so little reliable information on the most important issue of them all – how to reduce all-cause mortality.
In the rearview mirror, the effect of government interventions on excess mortality should hit us in the face – but it doesn’t.
Governments took extreme actions to counter COVID-19 on the grounds that it presented an extreme once-in-100 years threat that would impact everyone. The ICL COVID response Group’s Infamous Report 9 predicted it could lead to extraordinary levels of mortality (2.2 million in the US). They recommended a grand strategy (so to speak) of suppressing the virus until an effective vaccine came along, which it was implied would end the pandemic.
In response to this hypothetical scenario, governments panicked, ignored their own pandemic preparedness plans and adopted high-risk strategies that imposed restrictions on individual liberty never seen before. These countermeasures caused major harms and collateral damage, including loss of lives from delayed medical care and the medium-term aftereffects of increased unemployment and increased extreme poverty (for example the World Bank found that ‘the pandemic led to 97 million more people being in [extreme] poverty in 2020’).
But the ICL group’s estimates of mortality were based on preliminary data and dubious assumptions and were grossly overestimated. We can see this by comparing their early assumptions of the Infection Fatality Rate (IFR) with the retrospective calculations of the IFR by John Ioannidis and colleagues, based on hard data. The ICL report assumed a total IFR for all age groups of 0.9%, whereas Ioannidis found that the IFR for ages 0-59 was 0.07% and the figure for 0-69 was 0.09%.
| Age Group | ICL | Ioannidis |
| 20-29 | 0.03% | 0.003% |
| 30-39 | 0.08% | 0.011% |
| 40-49 | 0.15% | 0.035% |
| 50-59 | 0.6% | 0.129% |
| 60-69 | 2.2% | 0.501% |
So, we can see that the ICL estimates of mortality that led to the great lockdowns were at least ten times greater than the empirical outcomes. You can see why Ioannidis was first author of a paper entitled: ‘Forecasting has failed.’ And yet government policy was frequently guided by dodgy forecasting and modeling. The defense from the modeling groups is that they were not forecasting but generating scenarios. But government policy was driven by worst-case scenarios that were not plausible, and ICL went beyond generating scenarios to recommend the grand strategy.
So, government policy settings were based on information that was simply wrong. The underlying rationale that there was an extreme threat that necessitated extreme measures impacting the whole population was not valid.
In any case, there is no a priori reason to believe that extreme measures are more effective than moderate measures. Ioannidis and colleagues have again addressed this, finding that countries with more restrictive policies did not have lower case growth rates compared with countries with less restrictive policies.
Other strategies with a better cost-benefit ratio should have been considered. For example, a meta-analysis and systematic review by D’Ecclesiis et al. found ‘significant associations of vitamin D supplementation with Covid-19, encompassing risks of disease worsening and mortality, especially in seasons characterized by 25OHD deficiency and with not severe patients.’ Further, they found that supplementation with Vitamin D brought about a 55% reduction in disease severity.
The benefits of Vitamin D supplementation are greatest for those with deficiency, and long-term care facility populations are bound to have a high proportion of individuals deficient in Vitamin D. Even something as simple as nasal irrigation with saline should be further investigated. Baxter et al. concluded: ‘SARS-CoV-2+ participants initiating nasal irrigation were over 8 times less likely to be hospitalized than the national rate.’
Human rights law and public health law allow rights to be derogated temporarily in times of public emergency, but governments need to consider the alternatives and select the least restrictive strategies that will achieve the policy objective. But the policy objectives were unclear and kept shifting, and governments went straight for the harshest measures ever imposed on populations.
These issues have not been addressed in the major retrospective reviews of pandemic management so far. The high-profile group commissioned by The Lancet uncritically accepted the grand strategy of ‘suppression’ or ‘containment’ followed by vaccination, without considering the quality of the evidence behind it. While there is a good discussion of collateral damage in their report, their attempt at cost-benefit analysis is limited to a comparison between the estimated value of lives lost attributed to COVID-19 and the loss of GDP from containment measures.
This completely misses the high potential loss of life resulting from the collateral damage caused by the measures, including the well-known health impacts of unemployment and poverty. The Lancet Commission’s recommendations for future pandemic preparedness (p43) do not address the effectiveness or the full cost-benefit (in lives) of the grand strategy at all. See also this critique on Brownstone by David Bell.
Nature’s contribution was A multinational Delphi consensus to end the COVID-19 public health threat. These Delphic oracles also had an uncritical faith in ‘proven prevention measures,’ a key and questionable assumption on which all their recommendations rest and they had a strong focus on suppressing divergent perspectives.
By comparison, two Australian reviews were more probing, perhaps in reaction to their country’s extreme suppression policies and isolationism. The Shergold Review was commissioned by three philanthropic foundations and headed by a University Chancellor who was formerly the head of Australia’s public service.
This review focused on public policy and is highly critical of the ‘almost purposeful opaqueness of decision-making,’ finding that there was clear ‘overreach’ in the overreliance on extended lockdowns and border controls (perhaps emanating from the discredited former Prime Minister’s past triumph in suppressing unauthorized immigrants): ‘Our starting proposition should be that Australian citizens and permanent residents have a moral and human right to enter their own country.’ Turning back the waves of infection turned out to be more difficult than turning back the boats.
A group of public health experts also used a Delphi consensus approach to derive Key lessons from the COVID-19 public health response in Australia in a regional edition of The Lancet. This Group included experts who were widely quoted in the media and were the voice of reason through this period.
They too were highly critical of the extreme border control measures, and of the futility of the ‘zero-COVID’ strategy: ‘Once the SARS-CoV-2 virus was globally established (including in animal reservoirs), and given incomplete vaccine protection against virus transmission, it became clear that eradication (which was possible with SARS-CoV) was unachievable. The higher transmissibility of later SARS-CoV-2 variants and sub-variants, of concern made the pursuit of a zero COVID policy unattainable and incompatible with global connectedness.’
Here they have ‘zeroed in’ (so to speak) on a critical strategic issue that was evaded by the global retrospectives in Nature and the Lancet: once a respiratory spreads around the world, the case for containment and suppression becomes weak, and mitigation should be seriously considered. Governments profoundly overestimated their ability to shape the pandemic.
There will be more retrospective reviews, including by governments. They should revise their position on suppression virus mitigation, but they won’t. This key strategic choice will not be discussed. But lockdowns and vaccination mandates should not become normalized. Human rights should not be trampled on for such uncertain returns.
It is very unlikely that governments will take a truly strategic approach going forward, and much more likely that they will accept the orthodox ‘vaccination +’ model without considering other options. This leaves the door open to further overreach in future pandemics.
Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.