It is a tried-and-true tactic with effective and dastardly results. Big Pharma and other well-financed interests sponsor purportedly “impartial” medical trials aimed at discrediting cheaper generic alternatives. Ignoring the flaws in the methodology, the media runs wild with the desired narrative, which is amplified by a well-orchestrated public relations effort.
Social media shuts down alternative views and critiques. The result is fewer choices and higher prices for vaccines and anti-viral drugs—terrible for consumer health, but terrific for pharma companies’ bottom lines.
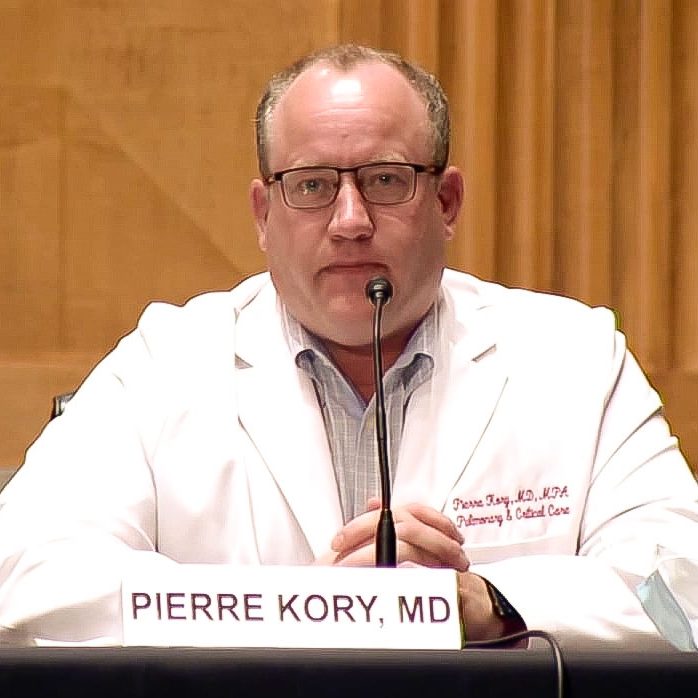
A newly reported clinical trial known as “TOGETHER,” ostensibly aimed at studying the effectiveness of ivermectin to treat Covid, perfectly illustrates the problem. To say the trial has many flaws is an understatement. To cite just a few, there were no explicit exclusion criteria for trial participants on ivermectin, meaning both trial groups had access to the same drug. This is an indefensible omission given that in Brazil, where the trial was conducted, ivermectin is available over-the-counter and widely used.
The treatment window was set for only three days, an obvious “tell” of underdosing given, for example, that both Merck’s molnupiravir and Pfizer’ Paxlovid require five days. The trial actually started out testing only a single dose, presumably until the investigators realized they could never disprove anything with that regimen.
And the trial was conducted during the throes of the massive gamma variant surge, one of the most virulent and deadly Covid variants. The dosage of the trial was far lower than everyday Brazilian clinicians were prescribing patients at the time to match the strength of the strain.
In spite of these and other readily apparent shortcomings, the nation’s leading media gobbled up the results. “Ivermectin Didn’t Reduce Covid-19 Hospitalizations in Largest Trial to Date” blared the Wall Street Journal, while a New York Times headlined announced, “Ivermectin Does Not Reduce Risk of Covid Hospitalization, Large Study Finds.”
Leading social media platforms took draconian measures to stifle follow-up conversation daring to question the company line. For example, clicking on a Reddit thread featuring MDs, PhDs and public health professionals discussing the randomization of the TOGETHER trial first brings users to an ominous page with a “quarantine” caveat, urging readers to “please consult your physician.” The most grotesque perversions imaginable are readily available to any child on the Internet, but informed medical conversations come with a warning label.
Unfortunately, the crackdowns do not stop there. California is pushing legislation (Assembly Bill 2098) to punish doctors who dare question phony studies. The proposed consequences are steep: loss of a medical license, every physician’s livelihood. If successful, other states will follow suit. This is extremely troubling for the practice of medicine.
Whatever other disagreements may arise over Covid, advancing access to medicines with the most effective treatment should be a universal goal. For ivermectin, a similar study of far larger size, conducted by investigators without any conflicts of interest, found the drug led to massive reductions in Covid infection, hospitalization and mortality—yet it received virtually no media coverage.
Moreover, cheaper and equally effective generic treatments such as fluvoxamine, with large trials published in the Lancet and JAMA showing positive results against Covid, fail to get recommendations from the agencies or medical societies
Ending this cycle of perpetual disinformation requires revamping our dysfunctional drug approval process. An independent board free of pharma industry conflicts must be established to oversee trials for re-purposed medicines. Recommendations should be based on trials designed by impartial experts and actual results, not the desired ones, and policymakers or prescribers who ignore the findings should be held accountable.
We must also remind academia and the regulatory agencies that observational trials data –wherein a sample of population who take a drug are compared to those who do not – is equally valid at informing policy. Randomized controlled trials can yield useful information, but their complexity, costs, and delays to treatment lead to errors and effectively shut out low-cost drugs from the approval process, regardless of their efficacy.
As part of their ongoing vigilance toward Covid, public health and elected officials are fond of saying the pandemic is not done with us. On that point, they are correct. Already, new Omicron variants are capturing media attention and starting a renewed debate over public health measures. Philadelphia has already re-imposed a mask mandate only to repeal it in response to public backlash. To combat new strains, we must turn our unbiased attention to repurposed drugs. Effectiveness, availability, and cost should be the guiding principles, not the bottom line of the big pharmaceutical companies.
Published under a Creative Commons Attribution 4.0 International License
For reprints, please set the canonical link back to the original Brownstone Institute Article and Author.